Visarpa Chikitsa
Chikitsa Sthana Chapter 21. Management of Visarpa (acute spreading erysepalas)
| Section/Chapter | Chikitsa Sthana Chapter 21 |
|---|---|
| Preceding Chapter | Chhardi Chikitsa |
| Succeeding Chapter | Trishna Chikitsa |
| Other Sections | Sutra Sthana, Nidana Sthana, Vimana Sthana, Sharira Sthana, Indriya Sthana, Kalpa Sthana, Siddhi Sthana |
| Translator and commentator | Kendre M. |
| Reviewer | Ojha S.N. |
| Editors | Ojha S.N., Deole Y.S., Basisht G. |
| Year of publication | 2020 |
| Publisher | Charak Samhita Research, Training and Skill Development Centre |
| DOI | 10.47468/CSNE.2020.e01.s06.022 |
Abstract
This chapter deals with detailed description of etiopathogenesis, classification and management principles of visarpa. This is acute disease with a quick spread involving mainly skin, blood, lymph and muscle tissue due to vitiation of all three dosha. Disease is clinically presented in three pathways viz. external, internal and both. Based on the involvement of dominant dosha, it is classified into seven types. Prognosis and treatment duration of disease is proportionate to degree of involvement of dosha and affected internal organs. As the basic nature of disease is rakta and pitta dominant, management is focused on body purification treatments especially therapeutic purgation, blood letting, fasting therapy, medicated ghee, use of bitter drugs and various external applications having soothing and cooling effect. Guidelines for external application in the form of pralepa, pradeha and alepa are enlisted in the chapter. Blood letting is emphasized as most important treatment in visarpa.
Keywords: Visarpa, Parisarpa, Erysepalas, Gangrene, Septicaemia, Sepsis, Fulminant spreading skin infections.
Introduction
The twenty first chapter is named Visarpa Chikitsa. The term visarpa has two parts viz., vi and sarpa- vi stands for vividha meaning ‘various’ (ways) and sarpa stands for sarpan means ‘spreading’. Erythematous, pustular, glandular etc. lesions which spread rapidly in localized or generalized pattern are known as visarpa [ Cha.Sa. Chikitsa Sthana 21/11, Chakrapani]. This aliment is also called parisarpa. The prefix pari stands for paritah or sarvatah meaning all over. The disease which spreads all over the body is called visarpa. [Cha. Sa.Chikitsa Sthana 21/11, Chakrapani]. This indicates that visarpa is an umbrella term used for acute spreading disorders caused due to vitiation of rakta.
In this chapter Atreya answers the queries about visarpa derivation, synonyms, classification, dosha, dushya, etiology, habitat, gradation, symptoms, complications, prognosis and treatment of curable ones. The chapter follows that of[ Cha. Sa. Chhardi Chikitsa ] because suppression of chhardi (vomiting) causes rakta dushti(vitiation of blood) leading to visarpa indicating that rakta (blood) vitiating factors and vitiation of rakta is an important basic underlying phenomenon prior to the visarpa.
Visarpa is acute, spreading and fatal in nature leading to death if not treated promptly. On location basis this is classified into bahih-shrita (externally situated), antah-shrita (internally situated) and ubhayasam shrita (all over situated). Bahih-shrita visarpa is fulminant, spreading skin and flesh infection with symptoms and signs of inflammatory edema, blisters, ulcers, fever, pain etc. and is curable. Antah-shrita visarpa involves internal vital organs with mild septicaemia and is curable before complications. Ubhayasamshrita visarpa has advanced manifestations of both types spreading all over body with severe septicaemia and is fatal.
Visarpa never occurs without association of rakta and pitta, hence general treatment of visarpa is described by considering rakta and pitta vitiation. Specific treatments are described by considering particular dosha involvement. Various etiological factors of visarpa are diet, life style, injury, poison, toxin, burn etc. vitiates rakta as well as dosha (vata, pitta and kapha) and other dhatu (body elements) leading to fulminant disease requiring urgent medical care.
Seven components are involved in the pathogenesis of visarpa viz., rakta (blood), lasika (lymph), tvak (skin), mamsa dhatu (flesh), vata, [[pitta and kapha. Same components are associated with kushtha (various skin disorders) but clinical presentation of both the diseases is different because etiological factors act different. As kushtha is chronic in nature and visarpa is acute in nature[Cha. Sa. Chikitsa Sthana 21/15,Chakrapani] therefore spreading kushtha should not be interpreted as visarpa.
It is also classified into vatika, paittika, slaishmika, agni visarpa, kardam visarpa, granthi visarpa and sannipatik on dosha basis. Bahih-shrita visarpa involves exterior part i.e. Skin, flesh, etc. of the body having symptoms like inflammatory oedema, blisters, ulcers, fever, pain etc. and is curable. Agni visarpa and kardam visarpa may be cured with appropriate timely management otherwise negligence leads to death of the patient. Granthi visarpa should be treated before complications otherwise it becomes incurable. Sannipatika visarpa is a severe manifestation of the disease leading to death.[Cha. Sa. Chikitsa Sthana 21/42]
In visarpa, shodhana therapy has given prime importance because rakta kleda (putrificatory ingredient) and dosha vitiation is at higher level hence samana (pacification) therapy is not very effective. Visarpa never occurs without association of rakta and pitta. Hence general treatment of visarpa is described by considering rakta and pitta vitiation. Specific treatments are described as per the involvement of dosha. Single raktamokshana (blood letting) treatment is equal to all of other treatments described for visarpa. [Cha. Sa. Chikitsa Sthana 21/141-143].
Kshataja visarpa is another variety mentioned additionally in Sushruta Samhita. The later texts followed the same description with addition of some medications.
Sanskrit Text, Transliteration and English Translation
Now we shall expound the chapter "Visarpa Chikitsa" (Management of acute spreading erysepalas). Thus said Lord Atreya. [1-2]
Agnivesha’s queries on visarpa
कैलासे किन्नराकीर्णे बहुप्रस्रवणौषधे |
पादपैर्विविधैः स्निग्धैर्नित्यं कुसुमसम्पदा ||३||
वमद्भिर्मधुरान् गन्धान् सर्वतः स्वभ्यलङ्कृते |
विहरन्तं जितात्मानमात्रेयमृषिवन्दितम् ||४||
महर्षिभिः परिवृतं सर्वभूतहिते रतम् |
अग्निवेशो गुरुं काले विनयादिदमुक्तवान् ||५||
भगवन्! दारुणं रोगमाशीविषविषोपमम् |
विसर्पन्तं शरीरेषु देहिनामुपलक्षये ||६||
सहसैव नरास्तेन परीताः शीघ्रकारिणा |
विनश्यन्त्यनुपक्रान्तास्तत्र नः संशयो महान् ||७||
स नाम्ना केन विज्ञेयः सञ्ज्ञितः केन हेतुना |
कतिभेदः कियद्धातुः किन्निदानः किमाश्रयः ||८||
सुखसाध्यः कृच्छ्रसाध्यो ज्ञेयो यश्चानुपक्रमः |
कथं कैर्लक्षणैः किं च भगवन्! तस्य भेषजम् ||९||
तदग्निवेशस्य वचः श्रुत्वाऽऽत्रेयः पुनर्वसुः |
यथावदखिलं सर्वं प्रोवाच मुनिसत्तमः ||१०||
In the Kailas region inhabited by kinnaras, having numerous water streams and medicinal plants with ever emitting sweet pleasant (ishat gandha) aroma by their wealth of flowers, Atreya who had great self-control, was surrounded by great sages and engaged in welfare of all creatures. Then Agnivesha choosing the appropriate time asked politely to his enlightened teacher, “Oh Lord, I observe the acute emergency disease in the body of human being which spreads with the virulence of snake-venom. Those human who are afflicted by this acute fulminating disease succumb to death quickly, unless treated promptly. We are in great need of enlightenment concerning this disease.
By which name should it be known? Why does it derive its name? What are its varieties? Which body elements are involved in its pathogenesis? What is its etiology? Where is its location? How to understand its prognosis i.e. easy curable, difficult to cure and incurable? What are the signs and symptoms of this disease? And O worshipful one! What is the method of its treatment?” Having heard the queries of Agnivesha, Atreya Punarvasu, the foremost among the sages, explained all the relevant details of the disease visarpa. [3-10]
Definition of visarpa
It spreads in various ways hence known as visarpa. It is also called parisarpa due to its extensive spreading.[11]
Classification
स च सप्तविधो दोषैर्विज्ञेयः सप्तधातुकः |
पृथक् त्रयस्त्रिभिश्चैको विसर्पो द्वन्द्वजास्त्रयः ||१२||
वातिकः पैत्तिकश्चैव कफजः सान्निपातिकः |
चत्वार एते विसर्पा वक्ष्यन्ते द्वन्द्वजास्त्रयः ||१३||
आग्नेयो वातपित्ताभ्यां ग्रन्थ्याख्यः कफवातजः |
यस्तु कर्दमको घोरः स पित्तकफसम्भवः ||१४||
Visarpa is of seven types as per dosha basis and it involves seven body elements.
Three types of visarpa are due to the morbidity of individual dosha; one variety is due to the morbidity of all the three dosha and three varieties are due to the morbidity of any of the two dosha.
Vatika, paittika, kaphaja and sannipatik these are the four varieties of visarpa and the remaining three varieties viz., vata-pittaja, kapha-vataja and pitta-kaphaja type will now be described.
The variety due to morbid vata-pitta is agnivisarpa, kapha-vata cause granthi visarpa and pitta-kapha leads to serious condition known as kardamaka visarpa. [12-14]
Vitiated factors
रक्तं लसीकात्वङ्मांसं दूष्यं दोषास्त्रयो मलाः |
विसर्पाणां समुत्पत्तौ विज्ञेयाः सप्त धातवः ||१५||
Blood, lymph, skin, flesh and three dosha, these seven elements are involved in the pathogenesis of visarpa of all kinds. [15]
Etiology
लवणाम्लकटष्णानां रसानामतिसेवनात् |
दध्यम्लमस्तुशुक्तानां सुरासौवीरकस्य च ||१६||
व्यापन्नबहुमद्योष्णरागषाडवसेवनात् |
शाकानां हरितानां च सेवनाच्च विदाहिनाम् ||१७||
कूर्चिकानां किलाटानां सेवनान्मन्दकस्य च |
दध्नः शाण्डाकिपूर्वाणामासुतानां च सेवनात् ||१८||
तिलमाषकुलत्थानां तैलानां पैष्टिकस्य च |
ग्राम्यानूपौदकानां च मांसानां लशुनस्य च ||१९||
प्रक्लिन्नानामसात्म्यानां विरुद्धानां च सेवनात् |
अत्यादानाद्दिवास्वप्नादजीर्णाध्यशनात् क्षतात् ||२०||
क्षतबन्धप्रपतनाद्धर्मकर्मातिसेवनात् [१] |
विषवाताग्निदोषाच्च विसर्पाणां समुद्भवः ||२१||
एतैर्निदानैर्व्यामिश्रैः कुपिता मारुतादयः |
दूष्यान् सन्दूष्य रक्तादीन् विसर्पन्त्यहिताशिनाम् ||२२||
The following are the causative factors of the visarpa:
Excessive indulgence in lavana (salt), amla (sour), katu (pungent) and ushna (hot ingredients); as also in amla dadhi (sour curd), dadhi mastu (whey), shukta (vinegars), sura (type of liquor) and sauviraka (type of wine); the use of vyapanna madya (contaminated wine) or excessive liquor or heat inducing raga (condiments) and sadava (confectionery), the use of vidahi (causes burning), shaka (vegetables) and harita (lashunadi harita group dravya), kilata (cheese), kurchika (inspissated milk) and mandaka (immature curd), the use of sandaki (fermented wine), as also of paistika (one made up of pistamai padarth or pastries) and oils made of sesame, black gram and horse gram, the use of flesh of domesticated, wet land and aquatic animals and garlic, the use of the praklinna (putrified food), asatmya (unwholesome) and viruddha (mutually contradictory ingredients), over eating, sleeping during day time, ajirnashana (eating during indigestion), adhyashana (eating food immediately after the meal); kshatat (traumatic injury), kshata (wounds), bandha (ligatures), prapatana (trauma due to falls) over exposure to sun, strainful work, poisons, poisonous air,burns etc.
By combination of above mentioned etiological factors, the provoked vatadi dosha affect the susceptible body elements such as rakta, lasika etc. and spread in the body in those indulged in unwholesome diet. [16-22]
Pathways of spreading the disease
बहिःश्रितः श्रितश्चान्तस्तथा चोभयसंश्रितः |
विसर्पो बलमेतेषां ज्ञेयं गुरु यथोत्तरम् ||२३||
बहिर्मार्गाश्रितं साध्यमसाध्यमुभयाश्रितम् |
विसर्पं दारुणं विद्यात् सुकृच्छ्रं त्वन्तराश्रयम् ||२४||
अन्तःप्रकुपिता दोषा विसर्पन्त्यन्तराश्रये |
बहिर्बहिःप्रकुपिताः सर्वत्रोभयसंश्रिताः ||२५||
Externally situated (pathogenesis in shakha, rasa dhatuand rakta dhatu), internally situated (pathogenesis in internal organs and other dhatu) and situated in both (externally as well as internally) pathways visarpa is to be known more and more serious consecutively.
Externally situated visarpa is curable, internally situated visarpa is very serious and difficult to cure whereas externally as well as internally situated type is incurable.
The humors provoked in internal regions spreads internally, if provoked in external regions spreads externally and if provoked in both regions spreads all over the body.[23-25]
Causes and features of internal and external visarpa
मर्मोपघातात् सम्मोहादयनानां विघट्टनात् |
तृष्णातियोगाद्वेगानां विषमाणां प्रवर्तनात् ||२६||
विद्याद्विसर्पमन्तर्जमाशु चाग्निबलक्षयात् |
अतो विपर्ययाद्बाह्यमन्यैर्विद्यात् स्वलक्षणैः ||२७||
Affliction of vital organs, impaired consciousness, impaired circulation, morbid thirst and impaired natural urges and sudden reduction in digestive as well as immune power of body is known as antah-visarpa. Bahih-visarpa should be understood by the external manifestations appearing on skin flesh etc. and by their own specific symptoms. [26-27]
Bad prognostic features
Visarpa manifesting with all signs and symptoms, having strong etiological factors, which is associated with formidable complications and that situates as well as affects vital parts, proves fatal.[28]
Etio-pathogeneis and clinical features of vata dominant visarpa
रूक्षोष्णैः केवलो वायुः पूरणैर्वा समावृतः |
प्रदुष्टो दूषयन् दूष्यान् विसर्पति यथाबलम् ||२९||
तस्य रूपाणि- भ्रमदवथुपिपासानिस्तोदशूलाङ्गमर्दोद्वेष्टनकम्पज्वरतमककासास्थिसन्धिभेदविश्लेषणवेपनारोचकाविपाकाश्चक्षुषोराकुलत्वमस्रागमनं पिपीलिकासञ्चार इव चाङ्गेषु, यस्मिंश्चावकाशे विसर्पो विसर्पति [१] सोऽवकाशः श्यावारुणाभासः श्वयथुमान् निस्तोदभेदशूलायामसङ्कोचहर्षस्फुरणैरतिमात्रं प्रपीड्यते, अनुपक्रान्तश्चोपचीयते शीघ्रभेदैः स्फोटकैस्तनुभिररुणाभैः श्यावैर्वा तनुविशदारुणाल्पास्रावैः, विबद्धवातमूत्रपुरीषश्च भवति, निदानोक्तानि चास्य नोपशेरते विपरीतानि चोपशेरत इति वातविसर्पः ||३०||
Vayu aggravated by ununctuous and hot ingredients or by the obstruction due to vitiated dosha, impairs the body elements and spreads in proportion to its strength.
Its signs and symptoms are giddiness, burning sensation, excessive thirst, pricking sensation, severe pain, body ache, cramps, shivering, fever, feeling of entering in darkness, cough, breaking and splitting pains in the bones and joints, looseness in joints, trembling, anorexia, indigestion, congestion of the eyes, lacrimation and paresthesia; the region where the inflammation is spreading becomes blackish and reddish in color and edematous. The patient suffers from severe pricking, splitting or aching pain in the part affected as also extension and contractions of the parts, horripilation and quivering. If not treated it gives rise to quick bursting small blackish or reddish blisters with thin clear reddish and scanty discharge. The patient also suffers from the retention of flatus, urine and feces. Etiological factors do not suit and the contrary ones suit the patient, this is vata dominant visarpa. [29-30]
Etio-pathogeneis and clinical features of pitta dominant visarpa
पित्तमुष्णोपचारेण विदाह्यम्लाशनैश्चितम् |
दूष्यान् सन्दूष्य धमनीः [१] पूरयन् वै विसर्पति ||३१||
तस्य रूपाणि- ज्वरस्तृष्णा मूर्च्छा मोहश्छर्दिररोचकोऽङ्गभेदः स्वेदोऽतिमात्रमन्तर्दाहः प्रलापः शिरोरुक् चक्षुषोराकुलत्वमस्वप्नमरतिर्भ्रमः शीतवातवारितर्षोऽतिमात्रं हरितहारिद्रनेत्रमूत्रवर्चस्त्वं हरितहारिद्ररूपदर्शनं च, यस्मिंश्चावकाशे विसर्पोऽनुसर्पति सोऽवकाशस्ताम्रहरितहारिद्रनीलकृष्णरक्तानां वर्णानामन्यतमं पुष्यति, सोत्सेधैश्चातिमात्रं दाहसम्भेदनपरीतैः स्फोटकैरुपचीयते तुल्यवर्णास्रावैश्चिरपाकैश्च, निदानोक्तानि चास्य नोपशेरते विपरीतानि चोपशेरत इति पित्तविसर्पः ||३२||
The pitta aggravated by the use of hot regimen, by eating irritant and sour foods vitiates the susceptible body elements and by feeling the vessels, begins to spread.
Its signs and symptoms are fever, morbid thirst, fainting, disturbed consciousness, vomiting, anorexia, breaking body ache, excessive perspiration, burning, delirium, headache, congestion of the eyes, insomnia, restlessness, giddiness, excessive desire for cold air and water. Greenish or yellowish coloration of eyes, urine and feces, objects visualizes green and yellow. In the region where the visarpa spreads, becomes coppery, greenish, yellowish, bluish, blackish, reddish color. Affected part becomes excessively edematous and full of pustules, having intense burning and tearing pain, suppurating quickly and discharging fluid of similar color.
The etiological factors do no suit and the contrary ones suit the patient. This is pitta dominant visarpa. [31-32]
Etio-pathogeneis and clinical features of kapha dominant visarpa
स्वाद्वम्ललवणस्निग्धगुर्वन्नस्वप्नसञ्चितः |
कफः सन्दूषयन् दूष्यान् कृच्छ्रमङ्गे विसर्पति ||३३||
तस्य रूपाणि- शीतकः शीतज्वरो गौरवं निद्रा तन्द्राऽरोचको मधुरास्यत्वमास्योपलेपो निष्ठीविका छर्दिरालस्यं स्तैमित्यमग्निनाशो दौर्बल्यं च, यस्मिंश्चावकाशे विसर्पोऽनुसर्पति सोऽवकाशः श्वयथुमान् पाण्डुर्नातिरक्तः स्नेहसुप्तिस्तम्भगौरवैरन्वितोऽल्पवेदनः कृच्छ्रपाकैश्चिरकारिभिर्बहुलत्वगुपलेपैः स्फोटः श्वेतपाण्डुभिरनुबध्यते, प्रभिन्नस्तु श्वेतं पिच्छिलं तन्तुमद्धनमनुबद्धं स्निग्धमास्रावं स्रवति, ऊर्ध्वं च गुरुभिः स्थिरैर्जालावततैः स्निग्धैर्बहुलत्वगुपलेपैर्व्रणैरनुबध्यतेऽनुषङ्गी च भवति, श्वेतनखनयनवदनत्वङ्मूत्रवर्चस्त्वं, निदानोक्तानि चास्य नोपशेरते विपरीतानि चोपशेरत इति श्लेष्मविसर्पः ||३४||
Kapha excessively accumulated due to intake of sweet, sour, salt, unctuous and heavy foods, and also by excessive sleep, vitiates the susceptible body elements and spreads with slow speed in the body.
Its signs and symptoms are chills, fever with chills, heaviness, excess sleep, drowsiness, adherence of sticky material in the mouth, excess spitting, vomiting, lassitude, timidity, loss of appetite and prostration. The region where the disease spreads becomes edematous, pallor or slight red, unctuous, numbness, rigidness, heaviness and slight pain. It suppurates hardly and chronic in nature. It is studded with eruptions which are covered with a thick skin and having white pale color. When burst, they discharge white, slimy, fibrinous, dense, sticky and viscid discharge from it. Thereafter it is followed by the ulcers which are heavy, deep seated, surrounded by capillary network, unctuous and covered with many skin scabs. These ulcers are chronic in nature. The nails, eyes, face, skin, urine and faces of the patient appear pale. The etiological factors do no suit and the contrary ones suit the patient. This is kaphaja visarpa. [33-34]
Etio-pathogenesis and clinical features of vata-pitta dominant agni visarpa
वातपित्तं प्रकुपितमतिमात्रं स्वहेतुभिः |
परस्परं लब्धबलं दहद्गात्रं विसर्पति ||३५||
तदुपतापादातुरः सर्वशरीरमङ्गारैरिवाकीर्यमाणं मन्यते, छर्द्यतीसारमूर्च्छादाहमोहज्वरतमकारोचकास्थिसन्धिभेदतृष्णाविपाकाङ्गभेदादिभिश्चाभिभूयते, यं यं चावकाशं विसर्पोऽनुसर्पति सोऽवकाशः शान्ताङ्गारप्रकाशोऽतिरक्तो वा भवति, अग्निदग्धप्रकारैश्च स्फोटैरुपचीयते, स शीघ्रगत्वादाश्वेव मर्मानुसारी भवति, मर्मणि चोपतप्ते पवनोऽतिबलो भिनत्त्यङ्गान्यतिमात्रं प्रमोहयति सञ्ज्ञां, हिक्काश्वासौ जनयति, नाशयति निद्रां, स नष्टनिद्रः प्रमूढसञ्ज्ञो व्यथितचेता न क्वचन सुखमुपलभते, अरतिपरीतः स्थानादासनाच्छय्यां क्रान्तुमिच्छति, क्लिष्टभूयिष्ठश्चाशु निद्रां भजति, दुर्बलो दुःखप्रबोधश्च भवति; तमेवंविधमग्निविसर्पपरीतमचिकित्स्यं विद्यात् ||३६||
When vata-pitta vitiated severely due to their respective etiological factors and strengthened mutually, spreads producing severe burning pain in the body.
The patient affected with this type of visarpa feels as if his body is sprinkled with flaming coals. He suffers from vomiting, diarrhea, fainting, burning sensation, disturbed consciousness, fever, feeling of darkness, anorexia, breaking pain in bones and joints, morbid thirst, indigestion, breaking body pain etc. The part where the disease spreads looks like extinguished charcoal or blood like red, affected region gets covered with blisters like those caused by burns. Due to its rapid progress, it soon spreads to vital regions. When the vital parts gets affected, the vata which is excessively aggravated causes extensive disintegration of the tissues and leads to disturbed consciousness, produces hiccup, dyspnea and insomnia. That sleepless patient with disturbed consciousness and miserable mind does not get relief anywhere. He becomes restless in standing, seating and desires to lie on bed, thus exceedingly exhausted due to pain soon falls into deep sleep. Being debilitated, he is aroused from this state with difficulty. One suffering from agni-visarpa is to be regarded as incurable.[35-36]
Etio-pathogenesis and clinical features of kapha-pitta dominant kardam visarpa
कफपित्तं प्रकुपित्तं बलवत् स्वेन हेतुना |
विसर्पत्येकदेशे तु प्रक्लेदयति देहिनम् ||३७||
तद्विकाराः- शीतज्वरः शिरोगुरुत्वं दाहः स्तैमित्यमङ्गावसदनं निद्रा तन्द्रा मोहोऽन्नद्वेषः प्रलापोऽग्निनाशो दौर्बल्यमस्थिभेदो मूर्च्छा पिपासा स्रोतसां प्रलेपो जाड्यमिन्द्रियाणां प्रायोपवेशनमङ्गविक्षेपोऽङ्गमर्दोऽरतिरौत्सुक्यं चोपजायते, प्रायश्चामाशये विसर्पत्यलसक एकदेशग्राही च, यस्मिंश्चावकाशे विसर्पो विसर्पति सोऽवकाशो रक्तपीतपाण्डुपिडकावकीर्ण इव मेचकाभः कालो मलिनः स्निग्धो बहूष्मा गुरुः स्तिमितवेदनः श्वयथुमान् गम्भीरपाको निरास्रावः शीघ्रक्लेदः स्विन्नक्लिन्नपूतिमांसत्वक् क्रमेणाल्परुक् परामृष्टोऽवदीर्यते कर्दम इवावपीडितोऽन्तरं प्रयच्छत्युपक्लिन्नपूतिमांसत्यागी सिरास्नायुसन्दर्शी कुणपगन्धी च भवति सञ्ज्ञास्मृतिहन्ता च; तं कर्दमविसर्पपरीतमचिकित्स्यं विद्यात् ||३८||
Excessively aggravated kapha pitta due to their respective etiological factors, spreads in the body causing suppuration of the tissues in particular part.
Its signs and symptoms are fever with chills, heaviness of the head, burning sensation, timidity, prostration, excessive sleep, drowsiness, disturbed consciousness, food dislike, delirium, loss of appetite, weakness, breaking pain in bones, fainting, morbid thirst, adhesions of sticky material in channels, dullness of the senses, mostly seating, abnormal movements of limbs, body pain, restlessness, anxiety, often it spreads to amashaya. It is localized and spreads with slow speed.
The part where the disease spreads looks as if filled with reddish, yellowish, pale eruptions. The affected part becomes muddy, black, dirty, unctuous, excess hot, heavy, dull aching, edematous, with deep seated suppuration, having no discharge, rapidly become sloughy, sweated suppurated, having putrid flesh and skin, gradual little pain, when touched bursts and gives space on pressing, throws out decomposed and putrefied flesh, shows blood vessels, ligaments and has cadaverous smell and causes disturbed consciousness as well as memory. This is called kardam visarpa and is incurable. [37-38]
Etio-pathogenesis and clinical features of kapha vata dominant granthi visarpa
स्थिरगुरुकठिनमधुरशीतस्निग्धान्नपानाभिष्यन्दिसेविनामव्यायामादिसेविनामप्रतिक र्मशीलानां श्लेष्मा वायुश्च प्रकोपमापद्यते, तावुभौ दुष्टप्रवृद्धावतिबलौ प्रदूष्य दूष्यान् विसर्पाय कल्पेते; तत्र वायुः श्लेष्मणा विबद्धमार्गस्तमेव श्लेष्माणमनेकधा भिन्दन् क्रमेण ग्रन्थिमालां कृच्छ्रपाकसाध्यां कफाशये सञ्जनयति, उत्सन्नरक्तस्य वा प्रदूष्य रक्तं सिरास्नायुमांसत्वगाश्रितं ग्रन्थीनां मालां कुरुते तीव्ररुजानां स्थूलानामणूनां वा दीर्घवृत्तरक्तानां, तदुपतापाज्ज्वरातिसारकासहिक्काश्वासशोषप्रमोहवैवर्ण्यारोचकाविपाकप्रसेकच्छ र्दिर्मूर्च्छाङ्गभङ्गनिद्रारतिसदनाद्याः प्रादुर्भवन्त्युपद्रवाः; स एतैरुपद्रुतः सर्वकर्मणां विषयमतिपतितो विवर्जनीयो भवतीति ग्रन्थिविसर्पः ||३९||
Kapha and vata gets vitiated due to the use of firm, heavy, hard, sweet, cold, unctuous, and abhishyandi (which increase discharges and cause obstruction) ingredients of diet, lack of physical exercise etc. not following preventive seasonal Panchakarma purification. Deranged excessively, aggravated, powerful both kapha and vata vitiates the susceptible body elements giving rise to granthi visarpa. Thereafter the vata being occluded by kapha in its progress and disintegrates kapha in many ways and gradually giving rise to chain of glands, hardly suppurating and difficult to cure, in the habitats of kapha.
In a person having aggravated blood, vitiated kapha-pitta provoke blood giving rise to a series of glandular enlargements which are exceedingly painful, large or small or elongated or round and of red color, located in blood vessels, ligaments, flesh and skin. Being afflicted, complications arise like fever, diarrhea, cough, hiccup, dyspnea, emaciation disturbed consciousness, abnormal complexion, anorexia, indigestion, excess salivation, vomiting, fainting, breaking pain in body , excessive sleep, restlessness, malaise, the patient associated with these complications goes beyond the reach of all remedial measures and as such is rejectable. This is granthi visarpa.[39]
Upadrava (complications)
उपद्रवस्तु खलु रोगोत्तरकालजो रोगाश्रयो रोग एव स्थूलोऽणुर्वा, रोगात् पश्चाज्जायत इत्युपद्रवसञ्ज्ञः| तत्र प्रधानो व्याधिः, व्याधेर्गुणभूत [१] उपद्रवः, तस्य प्रायः प्रधानप्रशमे प्रशमो भवति | स तु पीडाकरतरो भवति पश्चादुत्पद्यमानो व्याधिपरिक्लिष्टशरीरत्वात्; तस्मादुपद्रवं त्वरमाणोऽभिबाधेत ||४०||
Upadrava (complication) is disorder itself, outsized or undersized manifesting in the later period of a disease and rooted in the same (disease). Upadrava is so named because it manifests after the disease. Hence the main disease is primary and complication is secondary, it is generally pacified when the main disease gets pacified. It is more troublesome than the main disease itself, because it appears in the later stages of disease when the body is already weakened. Hence, one should treat the complications very promptly.[40]
Severity of visarpa
सर्वायतनसमुत्थं सर्वलिङ्गव्यापिनं सर्वधात्वनुसारिणमाशुकारिणं महात्ययिकमिति सन्निपातविसर्पमचिकित्स्यं विद्यात् ||४१||
The visarpa which is caused by all etiological factors, manifesting with all signs and symptoms, spreads in all body elements very rapidly and great disastrous is known as sannipataja visarpa and is not treatable. [41]
Prognosis of visarpa
तत्र वातपित्तश्लेष्मनिमित्ता विसर्पास्त्रयः साध्या भवन्ति; अग्निकर्दमाख्यौ पुनरनुपसृष्टे मर्मणि अनुपगते वा सिरास्नायुमांसक्लेदे साधारणक्रियाभिरुभावेवाभ्यस्यमानौ प्रशान्तिमापद्येयाताम्, अनादरोपक्रान्तः पुनस्तयोरन्यतरो हन्याद्देहमाश्वेवाशीविषवत्; तथा ग्रन्थिविसर्पमजातोपद्रवमारभेत चिकित्सितुम्, उपद्रवोपद्रुतं त्वेनं परिहरेत्; सन्निपातजं तु सर्वधात्वनुसारित्वादाशुकारित्वाद्विरुद्धोपक्रमत्वाच्चासाध्यं विद्यात् ||४२||
Among all types of visarpa vatik, paittik and kaphaja these three are curable. Agni and kardam visarpa not spreading to vital organs and causing no suppuration of the vessels, ligaments and muscles can be pacified by the general treatment of visarpa. When managed with negligence both may cause death of patients like snake venom. Granthi visarpa should be treated before complications has arisen, otherwise should be rejected. Sannipataja visarpa should be taken as incurable because of it is spreading to all dhatu, very fulminant and refractory to treatment.[42]
Principles of treatment
तत्र साध्यानां साधनमनुव्याख्यास्यामः ||४३||
लङ्घनोल्लेखने शस्ते तिक्तकानां च सेवनम् |
कफस्थानगते सामे रूक्षशीतैः प्रलेपयेत् ||४४||
पित्तस्थानगतेऽप्येतत् सामे कुर्याच्चिकित्सितम् |
शोणितस्यावसेकं च विरेकं च विशेषतः ||४५||
मारुताशयसम्भूतेऽप्यादितः स्याद्विरूक्षणम् |
रक्तपित्तान्वयेऽप्यादौ स्नेहनं न हितं मतम् ||४६||
वातोल्बणे तिक्तघृतं पैत्तिके च प्रशस्यते |
लघुदोषे, महादोषे पैत्तिके स्याद्विरेचनम् ||४७||
न घृतं बहुदोषाय देयं यन्न [१] विरेचयेत् |
तेन दोषो ह्युपष्टब्धस्त्वङ्मांसरुधिरं पचेत् ||४८||
तस्माद्विरेकमेवादौ शस्तं विद्याद्विसर्पिणः |
रुधिरस्यावसेकं च तद्ध्यस्याश्रयसञ्ज्ञितम् ||४९||
Now the treatment of the curable varieties of visarpa will be described.
If the visarpa is caused with ama dosha(dosha in the state of incomplete transformation) and is located in kaphasthana (in thorax and upper body parts), then langhana (fasting therapy), vamana (emesis) therapy, tikta (bitter) drugs internally and application of paste of drugs with dry and cold properties externally is beneficial.
The same treatment should be adopted in case of association of ama and location in pitta sthana (abdomen and middle parts of body).
In addition, raktamokshana (blood letting) and virechana (purgation therapy) are specially indicated.
If sama (with ama dosha) visarpa is arouse from vatashaya (pelvis and lower part of body) ununctuous measures are indicated in the beginning. Even in association with rakta-pitta uncting measure is not regarded as beneficial in the beginning.
In vataja visarpa and paittika visarpa of mild aggravated dosha tiktaka ghritam is beneficial. But if the pitta dosha is excessively aggravated then virechana should be given.
In the condition of excessively aggravated dosha, ghee should not be given at first which does not cause virechana. Because non purgating ghee occlude the dosha resulting in decomposed skin, flesh and blood. Hence in visarpa, virechana followed by raktamokshana is recommended because the disorder is located in blood.[43-49]
Formulations used in visarpa
इति वीसर्पनुत् प्रोक्तं समासेन चिकित्सितम् |
एतदेव पुनः सर्वं व्यासतः सम्प्रवक्ष्यते ||५०||
मदनं मधुकं निम्बं वत्सकस्य फलानि च |
वमनं सम्प्रदातव्यं विसर्पे कफपित्तजे ||५१||
पटोलपिचुमर्दाभ्यां पिप्पल्या मदनेन च |
विसर्पे वमनं शस्तं तथा चेन्द्रयवैः सह ||५२||
यांश्च योगान् प्रवक्ष्याभि कल्पेषु कफपित्तिनाम् |
विसर्पिणां प्रयोज्यास्ते दोषनिर्हरणाः शिवाः ||५३||
Thus the treatment principles of visarpa have been described in brief. The same is being detailed further.
In kapha pittaja visarpa, vamana should be given with the madana (Randia spinosa), madhuka (Glycyrrhiza glabra Linn), nimba (Azadirachta indica), and fruits of vatsaka (Holarrhena antidysenterica Linn).
In visarpa vamana is beneficial with patola (Trichosanthes dioica Roxb), pichumarda (Azadirachta indica), pippali (Piper longum linn), madana (Randia spinosa) and indrayava (Holarrhena antidysenterica Linn).
Further, all those formulations which will be described in kalpasthana in connection with the disorders of kapha pitta should be used for the patients of visarpa as well because they are eliminative of morbid dosha and are beneficial.[50-53]
मुस्तनिम्बपटोलानां चन्दनोत्पलयोरपि |
सारिवामलकोशीरमुस्तानां वा विचक्षणः ||५४||
कषायान् पाययेद्वैद्यः सिद्धान् वीसर्पनाशनान् |
किराततिक्तकं लोध्रं चन्दनं सदुरालभम् ||५५||
नागरं पद्मकिञ्जल्कमुत्पलं सबिभीतकम् |
मधुकं नागपुष्पं च दद्याद्वीसर्पशान्तये ||५६||
प्रपौण्डरीकं मधुकं पद्मकिञ्जल्कमुत्पलम् |
नागपुष्पं च लोध्रं च तेनैव विधिना पिबेत् ||५७||
द्राक्षां पर्पटकं शुण्ठीं गुडूचीं धन्वयासकम् |
निशापर्युषितं दद्यात्तृष्णावीसर्पशान्तये ||५८||
पटोलं पिचुमर्दं च दार्वीं कटुकरोहिणीम् |
यष्ट्याह्वां त्रायमाणां च दद्याद्वीसर्पशान्तये ||५९||
पटोलादिकषायं वा पिबेत्त्रिफलया सह |
मसूरविदलैर्युक्तं घृतमिश्रं प्रदापयेत् ||६०||
पटोलपत्रमुद्गानां रसमामलकस्य च |
पाययेत घृतोन्मिश्रं नरं वीसर्पपीडितम् ||६१||
The skillful physician should administer the decoctions of tested efficacy for the cure of visarpa made up of musta (Cyperus rotundus linn), nimba (Azadirachta indica) and patola (Trichosanthes dioica Roxb) or chandana (Santalum album linn) and utpal (Nymphaea nouchali) or sariva (Hemidesmus indicus), amalaki (Emblica officinalis), ushira (Vetiveria zizanioidis Linn) and musta (Cyperus rotundus linn).
Kiratatikta (Swertia chirayita), lodhra (Symplocos racemosa), chandana (Santalum album linn), duralabha (Fagonia cretica), shunthi (Zingiber officinale), padmakinjalka (Prunus cerasoides), utpala (Nymphaea nouchali), bibhitaka (Terminalia bellirica), madhuka (Glycyrrhiza glabra Linn) and nagapushpa (Mesua ferrea Linn), this formulation physician may administer for the alleviation of visarpa.
Prapaundrika (Nelumbo nucifera), madhuka (Glycyrrhiza glabra Linn), padmakinjalka (Prunus cerasoides), utpala (Nymphaea nouchali), nagapuspa (Mesua ferrea Linn), and lodhra (Symplocos racemosa), should be taken by the above method.
Draksha (Vitis vinifera Linn), parpataka (Carthmus tinctorius), shunthi (Zingiber officinale), guduchi (Tinospora cordifolia) and dhanvayasa (fagonia cretica) kept for the whole night in the water (shitakashaya), should be administered to alleviate morbid thirst and visarpa.
Patola (Trichosanthes dioica Roxb.), pichumarda (Azadirachta indica), darvi (Berberis aristata), katuki (Picrorhiza kurroa), rohini (Terminalia chebula), yasti (Glycyrrhiza glabra Linn.), and trayamana (Gentiana kurroo) should be administered to alleviate visarpa.
Physician should administer patoladi kashaya with triphala (Haritaki -Terminalia chebula, Bibhitaki-Terminalia bellirica, and amalaki- Emblica officinalis) and masur (lentil pulse) mixed with ghee.
Physician should administer patola patra (Trichosanthes dioica Roxb.), mudga (green gram) and amalaki juice (Emblica officinalis) mixed with ghee. [54-61]
Formulations for dosha situated in koshtha, pitta dominant visarpa and virechana
यच्च सर्पिर्महातिक्तं पित्तकुष्ठनिबर्हणम् |
निर्दिष्टं तदपि प्राज्ञो दद्याद्वीसर्पशान्तये ||६२||
त्रायमाणाघृतं सिद्धं गौल्मिके यदुदाहृतम् |
विसर्पाणां प्रशान्त्यर्थं दद्यात्तदपि बुद्धिमान् ||६३||
त्रिवृच्चूर्णं समालोड्य सर्पिषा पयसाऽपि वा |
घर्माम्बुना वा संयोज्य मृद्वीकानां रसेन वा ||६४||
विरेकार्थं प्रयोक्तव्यं सिद्धं वीसर्पनाशनम् |
त्रायमाणाशृतं वाऽपि पयो दद्याद्विरेचनम् ||६५||
त्रिफलारससंयुक्तं सर्पिस्त्रिवृतया सह |
प्रयोक्तव्यं विरेकार्थं विसर्पज्वरनाशनम् ||६६||
रसमामलकानां वा घृतमिश्रं प्रदापयेत् |
स एव गुरुकोष्ठाय त्रिवृच्चूर्णयुतो हितः ||६७||
दोषे कोष्ठगते भूय एतत् कुर्याच्चिकित्सितम् |68|
The mahatikta ghritam indicated in paittika kustha should also be given by the intelligent physician for the alleviation of visarpa.
Trayamana ghritam of tested efficacy mentioned in the treatment of gulma should be administered by the brilliant physician to alleviate visarpa.
The powder of trivritta (Operculina turpethum Linn) mixed with ghee or milk or hot water or mridvika (Vitis vinifera Linn) juice should be administered for virechana and is tested to alleviate visarpa or trayamana (Gentiana kurroo) decocted with milk should be given for virechana.
The decoction of triphala (Haritaki, Bibhitaki and Amalaki) mixed with ghee and trivritta (Operculina turpethum Linn) and used for virechana to alleviate visarpa and jwara.
The juice of amalaki (Emblica officinalis) mixed with ghee should be administered in visarpa patient of heavy bowel the same preparation mixed with trivritta (Operculina turpethum Linn) powder is beneficial.
When the morbid dosha are situated in kostha (internally), these measures should be administered.[62-67]
Formulations for dosha situated in shakha and modes of blood letting
शाखादुष्टे तु रुधिरे रक्तमेवादितो हरेत् ||६८||
भिषग्वातान्वितं रक्तं विषाणेन विनिर्हरेत् |
पित्तान्वितं जलौकोभिः, कफान्वितमलाबुभिः ||६९||
यथासन्नं विकारस्य व्यधयेदाशु वा सिराम् |
त्वङ्मांसस्नायुसङ्क्लेदो रक्तक्लेदाद्धि जायते ||७०||
If dosha in shakha (body elements) vitiate the blood then raktamokshana should be administered at first. The physician should use vishana (deer horn) in vata dominance, jalauka (Hirudinea medicinalis) in pitta dominance and alabu (lagenaria siceraria) in kapha dominance for blood letting or physician should perform siravyadha (blood letting through vein) promptly from the adjacent vein to the affected part, without which rakta kleda (putrifying blood content) gives rise to decomposed skin, flesh and ligaments. [68-70]
External applications
अन्तःशरीरे [१] संशुद्धे दोषे त्वङ्मांससंश्रिते |
आदितो वाऽल्पदोषाणां क्रिया बाह्या प्रवक्ष्यते ||७१||
उदुम्बरत्वङ्मधुकं पद्मकिञ्जल्कमुत्पलम् |
नागपुष्पं प्रियङ्गुश्च प्रदेहः सघृतो हितः ||७२||
न्यग्रोधपादास्तरुणाः कदलीगर्भसंयुताः |
बिसग्रन्थिश्च लेपः स्याच्छतधौतघृताप्लुतः ||७३||
कालीयं मधुकं हेम वन्यं चन्दनपद्मकौ |
एला मृणालं फलिनी प्रलेपः स्याद्धृताप्लुतः ||७४||
शाद्वलं च मृणालं च शङ्खं चन्दनमुत्पलम् |
वेतसस्य च मूलानि प्रदेहः स्यात् सतण्डुलः ||७५||
सारिवा पद्मकिञ्जल्कमुशीरं नीलमुत्पलम् |
मञ्जिष्ठा चन्दनं लोध्रमभया च प्रलेपनम् ||७६||
नलदं च हरेणुश्च लोध्रं मधुकपद्मकौ [२] |
दूर्वा सर्जरसश्चैव सघृतं स्यात् प्रलेपनम् ||७७||
यावकाः सक्तवश्चैव सर्पिषा सह योजिताः |
प्रदेहो मधुकं वीरा सघृता यवसक्तवः ||७८||
बलामुत्पलशालूकं वीरामगुरुचन्दनम् |
कुर्यादालेपनं वैद्यो मृणालं च बिसान्वितम् ||७९||
यवचूर्णं समधुकं सघृतं च प्रलेपनम् |
हरेणवो मसुराश्च समुद्गाः श्वेतशालयः ||८०||
पृथक् पृथक् प्रदेहाः स्युः सर्वे वा सर्पिषा सह |
पद्मिनीकर्दमः शीतो मौक्तिकं पिष्टमेव वा ||८१||
शङ्खः प्रवालः शुक्तिर्वा गैरिकं वा घृताप्लुतम् |
(पृथगेते प्रदेहाश्च हिता ज्ञेया विसर्पिणाम् [३] ) |
प्रपौण्डरीकं मधुकं बला शालूकमुत्पलम् ||८२||
न्यग्रोधपत्रदुग्धीके सघृतं स्यात् प्रलेपनम् |
बिसानि च मृणालं च सघृताश्च कशेरुकाः ||८३||
शतावरीविदार्योश्च कन्दौ धौतघृताप्लुतौ |
शैवालं नलमूलानि गोजिह्वा वृषकर्णिका ||८४||
इन्द्राणिशाकं सघृतं शिरीषत्वग्बलाघृतम् [४] |
न्यग्रोधोदुम्बरप्लक्षवेतसाश्वत्थपल्लवैः ||८५||
त्वक्कल्कैर्बहुसर्पिर्भिः शीतैरालेपनं हितम् |
प्रदेहाः सर्व एवैते वातपित्तोल्बणे [५] शुभाः ||८६||
सकफे [६] तु प्रवक्ष्यामि प्रदेहानपरान् हितान् |
त्रिफलां पद्मकोशीरं समङ्गां करवीरकम् ||८७||
नलमूलान्यनन्तां च प्रदेहमुपकल्पयेत् |
खदिरं सप्तपर्णं च मुस्तमारग्वधं धवम् ||८८||
कुरण्टकं देवदारु दद्यादालेपनं भिषक् |
आरग्वधस्य पत्राणि त्वचं श्लेष्मातकस्य च ||८९||
इन्द्राणिशाकं काकाह्वां शिरीषकुसुमानि च |
शैवालं नलमूलानि वीरां गन्धप्रियङ्गुकाम् ||९०||
त्रिफलां मधुकं वीरां शिरीषकुसुमानि च |
प्रपौण्डरीकं ह्रीबेरं दार्वीत्वङ्मधुकं बलाम् ||९१||
पृथगालेपनं कुर्याद्द्वन्द्वशः सर्वशोऽपि वा |
प्रदेहाः सर्व एवैते देयाः स्वल्पघृताप्लुताः ||९२||
वातपित्तोल्बणे ये तु प्रदेहास्ते घृताधिकाः |
घृतेन शतधौतेन प्रदिह्यात् केवलेन वा ||९३||
घृतमण्डेन शीतेन पयसा मधुकाम्बुना |
पञ्चवल्ककषायेण सेचयेच्छीतलेन वा ||९४||
वातासृक्पित्तबहुलं विसर्पं बहुशो भिषक् |
सेचनास्ते प्रदेहा ये त एव घृतसाधनाः ||९५||
ते चूर्णयोगा वीसर्पव्रणानामवचूर्णनाः |
दूर्वास्वरससिद्धं च घृतं स्याद्व्रणरोपणम् ||९६||
दार्वीत्वङूमधुकं लोध्रं केशरं चावचूर्णनम् |
पटोलः पिचुमर्दश्च त्रिफला मधुकोत्पले ||९७||
एतत् प्रक्षालनं सर्पिर्व्रणचूर्णं प्रलेपनम् |
प्रदेहाः सर्व एवैते कर्तव्याः सम्प्रसादनाः [१] ||९८||
After the body is cleansed internally (systemic) and morbid dosha remains in the skin and flesh (external tissues), or dosha morbidity is little, the external treatment to be carried out will now be described.
The bark of udumbara (Ficus glomerata), madhuka (Glycyrrhiza glabra Linn), padmakinjalka (Prunas cerasoides), utpala (Nymphaea nouchali), nagapuspa (Mesua ferrea Linn) and priyangu (Callicarpa macrophylla) mixed with ghee and applied externally as pradeha and is beneficial.
The tender adventitious roots of nyagrodha (Ficus bengalensis Linn), pith of kadali (Musa paradisiaca Linn.) and rhizome of lotus should be mixed with ghee washed hundred times and is applied externally as a lepa.
The kaliyaka (Santalum album Linn), madhuka (Glycyrrhiza glabra Linn), hema (calophyllum inophyllum), vanya (cyperus esculentus), chandana (Santalum album Linn), padmaka (Prunas cerasoides), ela (Elettaria cardamomum), mrnala (Nelumbo nucifera) and phalini (Callicarpa macrophylla) should be mixed with ghee and is applied externally as a pralepa.
The roots shadvala (Elymus repens), mrnala (Nelumbo nucifera), shankha (conch shells), chandana (Santalum album Linn), utpala (Nymphaea nouchali), vetas (Salix caprea Linn) and tandula (rice) should be applied externally as a pradeha. Sariva (Hemidesmus indicus), padmakinjalka (Prunas cerasoides), ushira (Vetiveria zizanioidis), nila utpala (Nymphaea caerulea), manjistha (Rubia cordifolia), chandana (Santalum album Linn), lodhra (symplocos racemosa) and abhaya (Terminalia chebula) should be applied externally as pralepa.
Nalada (Vetiveria zizanioidis), harenu (Vitex negundo Linn), lodhra (Symplocos racemosa), madhuka (Glycyrrhiza glabra Linn), padmaka (Prunas cerasoides), durva (Cynodon dactylon) and sarjarasa (Shorea robusta) should be mixed with ghee and used externally as a pralepa.
The gruel prepared of barley or roasted flour of cereals should be mixed with ghee and also madhuka (Glycyrrhiza glabra Linn), vira (Pueraria tuberose) and yavasaktu mixed with ghee should be used externally as a pradeha.
The physician should use mixture of bala (Sida cordifolia Linn), utpala (Nymphaea nouchali), shaluka (Asparagus racemosus), vira (Pueraria tuberose), aguru (Aquilaria agallocha), chandana (Santalum album Linn), mrnala (stalk) and bisa (tubers of Nelumbo nucifera) externally as alepan (local application as a smear or thick paste or coating).
The powder of barley mixed with honey and ghee should be used externally as a pralepa (application as thin paste).
Harenu (Pisum sativum), masura (Lens culinaris), mudga (Vigna radiata) and white shali rice should be mixed with ghee individually or in combination and used externally as a pradeha (application as a poultice).
The cooling mud at the root of lotus, pearls or rice flour or conch shells, coral, oyster shell and ochre should be mixed with ghee separately and beneficial externally as a pradeha in visarpa.
Prapaundarika (Nelumbo nucifera), madhuka (Glycyrrhiza glabra Linn), bala (Sida cordifolia), shaluka (Asparagus racemosus), utpala (Nymphaea nouchali), nyagrodha (Ficus bengalensis Linn) and dugdhika (Euphorbia hirta Linn.) mixed with ghee should be used externally as a pralepan.
The bisa (lotus fibres), mrnala (lotus stalks) and kasheruka (Cyperus esculentus) mixed with ghee. The shatavari (Asparagus racemosus) and vidarikand (Pueraria tuberose) mixed with washed ghee.
The shaival (moss), root of nala (phragmites australis), gojihva (Amorphophallus paeoniifolius), vrsa karnika (Calystegia soldanella) and indranishaka (Vitex agnus-castus) mixed with ghee.
The bark of sirisa (Albizzia lebbeck) and bala (Sida cordifolia Linn) mixed with ghee. Nyagrodha (Ficus bengalensis Linn), udumbar (Ficus glomerata), plaksha (Ficus sycomorus), vetas (Salix caprea Linn), asvattha (Ficus religiosa) leaves and bark mixed with ample ghee used as a cold alepan is beneficial.
All these external applications are beneficial in vata pitta predominant visarpa.
Other external applications useful in kapha predominant visarpa will be described here after. Triphala (haritaki, bibhitaki and amalaki), padmaka (Prunas cerasoides), usir (Vetiveria zizanioidis Linn), samanga (Mimosa pudica), karviraka (Nerium indicum), root of nala (Phragmites australis) and ananta (hemidesmus indicus) should be used externally as a pradeha.
Khadira (Acacia catechu), saptaparna (Alstonia scholaris), musta (Cyperus rotundus linn), aragvadha (Cassia fistula Linn), dhava (Anogeissus latifolia, Wall). Kurantaka (Lawsonia inermis) and devdaru (Cedrus deodar) should be applied externally as a pradeha.
Aragvadha leaves (Cassia fistula Linn.) and sleshmantak bark (Cordia dichotoma), indrani shak (Vitex negundo Linn), kakahva (Canvalia gladiata) and sirisa flowers (Albizia lebbeck Linn.), saivala (Spirogyra maxima) root of nala (Phragmites australis), veera (Pueraria tuberose) and gandpriyangu (Callicarpa macrophylla), triphala (Haritaki, Bibhitaki and Amalaki), madhuka (Glycyrrhiza glabra Linn), prapaundrika (nelumbo nucifera), hribera (Pavonia odorata), bark of darvi (Berberis aristata), and bala (Sida cordifolia Linn.) - these should be applied singly, dually or collectively as a pradeha. All these external applications should be mixed with small quantity of ghee. In vata pitta predominant condition these preparations should be mixed with profuse quantity of ghee.
The applications of shatdhaut ghrita as pradeha or effuse with cold ghee scum, or cold milk or cold decoction of madhuka (Glycyrrhiza glabra Linn), or panchavalka (bark of nygrodha, udumbara, asvattha, plaksa and vetasa), the physician should use frequently in vata, rakta and pitta predominant visarpa.
The external application mentioned as pradeha may also be used for sprinkling or for preparation ghrita yoga or churna yoga used for dusting in wounds of visarpa, ghee cooked with durva juice promotes wound healing.
Bark of daruharidra (Berberis aristata), madhuka (Glycyrrhiza glabra Linn), lodhra (Symplocos racemosa) and keshara (Crocus sativus Linn), powder may be used for dusting the ulcers. Patola (Trichosanthes dioica Roxb), pichumarda (Azadirachta indica), triphala (haritaki, bibhitaki and amalaki), madhuka (Glycyrrhiza glabra Linn) and utpala (Nymphaea nouchali), these ingredients may be used to prepare decoction for cleansing the ulcers or to prepare ghrita or to prepare powder for dusting the ulcers or to prepare pralepa.
All these external applications as pradeha should be used for samprasadana (cleansing and pacifying the blood). [71-98]
Guidelines for local application and its types
क्षणे क्षणे प्रयोक्तव्याः पूर्वमुद्धृत्य लेपनम् |
अधावनोद्धृते पूर्वे प्रदेहा बहुशोऽघनाः ||९९||
देयाः प्रदेहाः कफजे पर्याधानोद्धृते घनाः |
त्रिभागाङ्गुष्ठमात्रः स्यात् प्रलेपः कल्कपेषितः ||१००||
नातिस्निग्धो न रूक्षश्च न पिण्डो न द्रवः समः |
न च पर्युषितं लेपं कदाचिदवचारयेत् ||१०१||
न च तेनैव लेपेन पुनर्जातु प्रलेपयेत् |
क्लेदवीसर्पशूलानि सोष्णाभावात् प्रवर्तयेत् ||१०२||
लेपो ह्युपरि पट्टस्य कृतः स्वेदयति व्रणम् |
स्वेदजाः पिडकास्तस्य कण्डूश्चैवोपजायते ||१०३||
उपर्युपरि लेपस्य लेपो यद्यवचार्यते |
तानेव दोषाञ्जनयेत् पट्टस्योपरि यान् कृतः ||१०४||
अतिस्निग्धोऽतिद्रवश्च लेपो यद्यवचार्यते |
त्वचि न श्लिष्यते सम्यङ्न दोषं शमयत्यपि ||१०५||
तन्वालिप्तं न कुर्वीत संशुष्को ह्यापुटायते |
न चौषधिरसो व्याधिं प्राप्नोत्यपि च शुष्यति ||१०६||
तन्वालिप्तेन ये दोषास्तानेव जनयेद्भृशम् |
संशुष्कः पीडयेद्व्याधिं निःस्नेहो ह्यवचारितः ||१०७||
These lepa (local applications of pastes) are to be used repeatedly after removing the previous applied lepa.
Thin predeha should be applied as thick paste repeatedly after removing the previous one, but without washing it.
In kaphaja visarpa, pradeha should be repeatedly applied as thick paste after removing the previous dried paste.
The pralepa should be prepared as kalka (micronized paste) and applied of thickness equal to one third of the thumb.
A pralepa should be neither too unctuous nor too dry, neither too solid nor too liquid, but of the right consistency.
The stale lepa should never be used for application; the previously used lepa should not be used again for application, because it causes accumulation of heat leading to kleda (putrification), visarpa (spread of disease) and pain.
The pralepa smeared over a piece of cloth, and that cloth is used for application on wound, it sudates the wound and consequently swedaja pidaka (boils) and itching are induced.
If the pralepa is applied without removing the previous pralepa, it produces same adverse effects as those mentioned above in the case of applications over the bandage.
The pralepa applied externally that is either too unctuous or too fluid does not adhere properly and therefore cannot alleviate the diseased condition.
Thin lepa should not be applied because while drying develops cracks and medicinal property of lepa does not penetrates properly in the affected part as it dries up quickly.
If the pralepa is applied without mixing ghee, it produces same but in excess adverse effects as described for thin pralepa. While getting dried up this pralepa leads to aggravation of disease manifestation. [99-107]
Diet recipes for treatment of visarpa
अन्नपानानि वक्ष्यामि विसर्पाणां निवृत्तये |
लङ्घितेभ्यो हितो मन्थो रूक्षः सक्षौद्रशर्करः ||१०८||
मधुरः किञ्चिदम्लो वा दाडिमामलकान्वितः |
सपरूषकमृद्वीकः सखर्जूरः शृताम्बुना ||१०९||
तर्पणैर्यवशालीनां सस्नेहा चावलेहिका |
जीर्णे पुराणशालीनां यूषैर्भुञ्जीत भोजनम् ||११०||
मुद्गान्मसूरांश्चणकान् यूषार्थमुपकल्पयेत् |
अनम्लान् दाडिमाम्लान् वा पटोलामलकैः सह ||१११||
जाङ्गलानां च मांसानां रसांस्तस्योपकल्पयेत् |
रूक्षान् परूषकद्राक्षादाडिमामलकान्वितान् ||११२||
रक्ताः श्वेता महाह्वाश्च शालयः षष्टिकैः सह |
भोजनार्थे प्रशस्यन्ते पुराणाः सुपरिस्रुताः ||११३||
यवगोधूमशालीनां सात्म्यान्येव प्रदापयेत् |
येषां नात्युचितः शालिर्नरा ये च कफाधिकाः ||११४||
The diet regimen helps to alleviate visarpa is described here after.
In the beginning langhana (fasting therapy) should be given. There after use of mantha (roasted flour mixed with water in specific proportion and kept for specific time) is beneficial. The mantha should be without unctus ingredients and added with honey and sugar. It becomes sweet sour in taste due to mixing of dadima (Punica granatum Linn.) or amalaki (Emblica officinalis) and parushaka or mrdvika (Vitis vinifera Linn) or kharjura (Phoenix sylvestris) and boiled water should be used to prepare mantha.
Thereafter linctus made of the flour of roasted barley and shali rice and mixed with ghee should be given in the form of avalehika. After digestion of avalehika, one should take old shali rice with soup of green gram or lentils or Bengal gram, soured or not soured with pomegranates and added with patola (Trichosanthes dioica Roxb) and amalaki. He may also take meat soup of wild animals without ghee and added with parushaka or draksha or dadima or amalaki. Red or white or extra long variety of shastika rice, which are old, well boiled and residual water should be completely drained, it is beneficial food.
The persons who have predominance of kapha and not suited to rice should be given the preparation of barley or wheat or purana shali which is suitable.[108-114]
Contra-indications in visarpa
विदाहीन्यन्नपानानि विरुद्धं स्वपनं दिवा |
क्रोधव्यायामसूर्याग्निप्रवातांश्च विवर्जयेत् ||११५||
The patient should avoid the vidahi (that causes burning) and viruddha (mutually contradictory or incompatible) diet, day sleep, anger, exercise, exposure to sun heat, fire and fast winds.[115]
General guidelines of treatment
कुर्याच्चिकित्सितादस्माच्छीतप्रायाणि पैत्तिके |
रूक्षप्रायाणि कफजे स्नैहिकान्यनिलात्मके ||११६||
वातपित्तप्रशमनमग्निवीसर्पणे हितम् |
कफपित्तप्रशमनं प्रायः कर्दमसञ्ज्ञिते ||११७||
Of these measures, predominantly sheeta (cool) measures are prescribed in pitta dominant condition, ruksha in kapha dominant condition and snigdha in vata dominant condition of visarpa.
In agni visarpa, vata-pitta pacifying measures are beneficial and in kardama visarpa mostly kapha pitta alleviating measures should be administered.[116-117]
Treatment of granthi visarpa
रक्तपित्तोत्तरं दृष्ट्वा ग्रन्थिवीसर्पमादितः |
रूक्षणैर्लङ्घनैः सेकैः प्रदेहैः पाञ्चवल्कलैः ||११८||
सिरामोक्षैर्जलौकोभिर्वमनैः सविरेचनैः |
घृतैः कषायतिक्तैश्च कालज्ञः समुपाचरेत् ||११९||
ऊर्ध्वं चाधश्च शुद्धाय रक्ते चाप्यवसेचिते |
वातश्लेष्महरं कर्म ग्रन्थिवीसर्पिणे हितम् ||१२०||
उत्कारिकाभिरुष्णाभिरुपनाहःप्रशस्यते|
स्निग्धाभिर्वेशवारैर्वा ग्रन्थिवीसर्पशूलिनाम् ||१२१||
दशमूलोपसिद्धेन तैलेनोष्णेन सेचयेत् |
कुष्ठतैलेन चोष्णेन पाक्यक्षारयुतेन च ||१२२||
गोमूत्रैः पत्रनिर्यूहैरुष्णैर्वा परिषेचयेत् |
सुखोष्णया प्रदिह्याद्वा पिष्टया चाश्वगन्धया ||१२३||
शुष्कमूलककल्केन नक्तमालत्वचाऽपि वा |
बिभीतकत्वचां वाऽपि कल्केनोष्णेन लेपयेत् ||१२४||
बलां नागबलां पथ्यां भूर्जग्रन्थिं बिभीतकम् |
वंशपत्राण्यग्निमन्थं कुर्याद्ग्रन्थिप्रलेपनम् ||१२५||
दन्ती चित्रकमूलत्वक् सुधार्कपयसी गुडः |
भल्लातकास्थि कासीसं लेपो भिन्द्याच्छिलामपि ||१२६||
बहिर्मार्गास्थितं ग्रन्थिं किं पुनः कफसम्भवम् |
दीर्घकालस्थितं ग्रन्थिं भिन्द्याद्वा भेषजैरिमैः ||१२७||
मूलकानां कुलत्थानां यूषैः सक्षारदाडिमैः |
गोधूमान्नैर्यवान्नैर्वा ससीधुमधुशर्करैः ||१२८||
सक्षौद्रेर्वारुणीमण्डैर्मातुलुङ्गरसान्वितैः |
त्रिफलायाः प्रयोगैश्च पिप्पलीक्षौद्रसंयुतैः ||१२९||
मुस्तभल्लातशक्तूनां प्रयोगैर्माक्षिकस्य च |
देवदारुगुडूच्योश्च प्रयोगैर्गिरिजस्य च ||१३०||
धूमैर्विरेकैः शिरसः पूर्वोक्तैर्गुल्मभेदनैः |
अयोलवणपाषाणहेमताम्रप्रपीडनैः ||१३१||
आभिः क्रियाभिः सिद्धाभिर्विविधाभिर्बली स्थिरः |
ग्रन्थिः पाषाणकठिनो यदा नैवोपशाम्यति ||१३२||
अथास्य दाहः क्षारेण शरैर्हेम्नाऽथ वा हितः |
पाकिभिः पाचयित्वा वा पाटयित्वा समुद्धरेत् ||१३३||
मोक्षयेद्बहुशश्चास्य रक्तमुत्क्लेशमागतम् |
पुनश्चापहृते रक्ते वातश्लेष्मजिदौषधम् ||१३४||
धूमो विरेकः शिरसः स्वेदनं परिमर्दनम् |
अप्रशाम्यति दोषे च पाचनं वा प्रशस्यते ||१३५||
प्रक्लिन्नं दाहपाकाभ्यां भिषक् शोधनरोपणैः |
बाह्यैश्चाभ्यन्तरैश्चैव व्रणवत् समुपाचरेत् ||१३६||
कम्पिल्लकं विडङ्गानि दार्वीं कारञ्जकं फलम् |
पिष्ट्वा तैलं विपक्तव्यं ग्रन्थिव्रणचिकित्सितम् ||१३७||
द्विव्रणीयोपदिष्टेन कर्मणा चाप्युपाचरेत् |
देशकालविभागज्ञो व्रणान् वीसर्पजान् बुधः ||१३८||
इति ग्रन्थिविसर्पचिकित्सा |
The granthi visarpa, on inspection is predominant in rakta pitta; the physician experienced in timely management should treat the case with rukshana (de-oleation), langhana (lightening therapy), seka (affusion), and pradeha (external application) of panchavalka, siramoksha (blood letting), jalauka (leech therapy), vamana (emesis therapy), virechana (purgation therapy) and kashaya- tikta (astringent and bitter) ghee preparations.
After cleansing of body by vamana and virechana, rakta mokshana should be administered and the measures alleviating vata-kapha are beneficial.
When there is pain in granthi visarpa, upanaha (hot poultice) of warm and unctuous utkarika (medicinal pancake) or vesavara (medicated meat) application on the affected part is beneficial.
The warm oil prepared from dashamoola (roots of ten plants) should be sprinkled on the affected part. Warm kustha (costus) oil added with pakya kshara (prepared medicinal alkali) or warm cow’s urine or decoction of vata kaphahara leaves should be used as affusion on the affected part.
The warm paste of ashvagandha (Withania somnifera) should be applied as pradeha on the affected part.
The warm paste of dried mulaka (Raphanus sativus) or bark of naktamala (Pongamia pinnata) or bark of bibhitaka (Terminalia bellirica) should be applied externally as a lepa on the affected part. Bala (Sida cordifolia Linn), nagabala (Grewia hirsuta), pathya (Terminalia chebula), bhurjagranthi (betula bhojpatra), bibhitaka (Terminalia bellirica), vamsha leaves (bambusa vulgaris) and agnimantha (Premna mucronata) should be applied as pralepa on granthi.
Danti (Baliospermum montanum), bark of chitraka root (Plumbago zeylanica Linn), latex of snuhi (Euphoria nerrifolia) and arka (Calatropis gigantean), jaggery, seed of bhallataka (Semecarpus anacardium linn) and kasisa (green vitriol) application as a lepa breaks even a stone, then what to speak of the nodules caused by kapha and situated in external regions of body. Long standing granthi should be broken by the use of the internal medications such as Yusha of mulaka (Raphanus sativus) and kullatha (Macrotyloma uniflorum.) added with kshara (prepared alkali) and dadima (Punica granatum), food prepared from godhum and yava with sidhu, honey and sugar, varuni scum with honey and matulung juice (Citrus medica), use of triphala with pippali (Piper longum linn) and honey, musta (Cyperus rotundus linn) or bhallataka saktu (Semecarpus anacardium linn) and honey, devadaru (Cedrus deodara), guduchi (Tinospora cordifolia) and girija (Asphaltum punjabianum).
Dhuma, shirovirechana, measures described to break the gulma in Gulma Chikitsa chapter, as well as iron, salt, stone, gold and copper should be used for prapidana (compression) of granthi.
If granthi is strong, firm and stony hard and not responding to all these proven methods of treatment then it is better to be cauterized with kshara (medicinal alkali) or hot metal arrow or hot gold or after making it suppurate by applying suitable suppurative medications one should open and extract.
Besides, vitiated blood should be eliminated, frequently followed administration of vata and kapha pacifying medicines, dhuma (fumigation therapy), shirovechana (errhine therapy), swedana(sudation) and parimardana (pressure method). If dosha do not pacify, pachana (suppuration) treatment is beneficial. When the granthi is decomposed with agni and suppuration then physician should treat it with external and internal shodhana (cleansing) and ropana (healing) as described in Vrana Chikitsa.
Kampillaka (Mallotus philippinensis), vidanga (Embelia ribes Burm), daruharidra (Berberis aristata) and karanja fruit (Pongamia pinnata), the paste of all these drugs should be used to prepare oil which is indicated in the treatment of granthi vrina.
The intelligent physician may also treat the visarpa as per the guidelines described in Dwivraniya Chikitsa chapter.
Thus ends the description of the treatment of granthi visarpa.[118-138]
Treatment of galaganda
य एव विधिरुद्दिष्टो ग्रन्थीनां विनिवृत्तये |
स एव गलगण्डानां कफजानां निवृत्तये ||१३९||
गलगण्डास्तु वातोत्था ये कफानुगता नृणाम् |
घृतक्षीरकषायाणामभ्यासान्न भवन्ति ते ||१४०||
The line of treatment of granthi should be applied for the treatment of kaphaja galganda.
The vatika galaganda associated with kapha may be cured by regular use of ghee, milk and decoction preparations.[139-140]
Importance of raktamokshana in visarpa
यानीहोक्तानि कर्माणि विसर्पाणां निवृत्तये |
एकतस्तानि सर्वाणि रक्तमोक्षणमेकतः ||१४१||
विसर्पो न ह्यसंसृष्टो रक्तपित्तेन जायते |
तस्मात् साधारणं सर्वमुक्तमेतच्चिकित्सितम् ||१४२||
विशेषो दोषवैषम्यान्न च नोक्तः समासतः |
समासव्यासनिर्दिष्टां क्रियां विद्वानुपाचरेत् ||१४३||
If all the therapeutic measures described here as curative of visarpa be put on one side and raktamokshana on other, they will be found equal.
Visarpa never occurs without the association of the rakta and pitta hence entirely general treatment has been described. It does not mean that line of treatment as per other dosha predominance is not explained here. Thus, the therapeutic measures both in general and specific cases are described both in brief and in detail. The expert physician should administer these therapies appropriately.[141-143]
Summary
तत्र श्लोकाः-
निरुक्तं नामभेदाश्च दोषा दूष्याणि हेतवः |
आश्रयो मार्गतश्चैव विसर्पगुरुलाघवम् ||१४४||
लिङ्गान्युपद्रवा ये च यल्लक्षण उपद्रवः |
साध्यत्वं, न च, साध्यानां साधनं च यथाक्रमम् ||१४५||
इति पिप्रक्षवे सिद्धिमग्निवेशाय धीमते |
पुनर्वसुरुवाचेदं विसर्पाणां चिकित्सितम् ||१४६||
Now the summing up verses –
Derivation,synonyms, classification, dosha, dushya, etiology, the habitat, the severe and mild gradation, symptoms and signs, complications, the nature of complications, prognosis and treatment of curable ones. All these aspects has been explained by Punarvasu Atreya for the inquisitive and intelligent Agnivesha under the treatment of visarpa. [144-146]
इत्यग्निवेशकृते तन्त्रे चरकप्रतिसंस्कृते चिकित्सास्थाने
विसर्पचिकित्सितं नामैकविंशोऽध्यायः ||२१||
Thus ends the twenty first chapter on treatment of visarpa in Chikitsa Sthana in the treatise composed by Agnivesha and redacted by Charak.[21]
Tattva Vimarsha (Fundamental Principles)
- Seven elements are involved in the pathogenesis of visarpa viz., rakta, lasika, tvak, mamsa dhatu, vata, pitta and kapha.
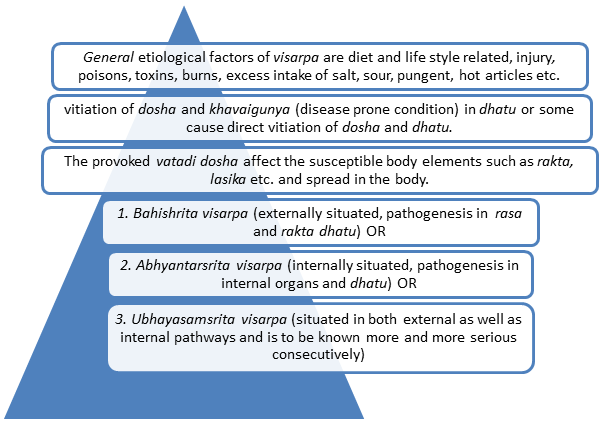
- Visarpa is acute spreading disease and fatal in nature. General etiological factors of visarpa are diet and life style related, injury, poisons, toxins, burns etc., some of these cause vitiation of dosha and khavaigunya (disease prone condition) in dhatu and some cause direct vitiation of dosha and dhatu leading to visarpa. Hence favorable condition for infection or disease phenomenon occurs at first therefore, diet and lifestyle related factors are important preventive measures.
- Excess intake of salt, sour, pungent, hot articles lead to vitiation of rakta first and then lead to visarpa.
- Visarpa is manifested externally, internally or in both pathways. Severity of disease increases respectively in these cases.
- Classification and pathogenesis of visarpa is based upon involvement of dosha as per their severity. Treatment protocol is designed for primarily involved predominant dosha. If the visarpa is caused with ama dosha (the state of incomplete transformation) and is located in kaphasthana (in thorax and upper body parts), then langhana (fasting therapy), vamana (emesis) therapy, tikta (bitter) drugs internally and application of paste of drugs with dry and cold properties externally is beneficial.
- The same treatment should be adopted in case of association of ama and location in pitta sthana (abdomen and middle parts of body). In addition, raktamokshana (blood letting) and virechana (therapeutic purgation therapy) are specially indicated.
- If sama (with ama dosha) visarpa occurs from vatashaya (pelvis and lower part of body) dry measures are indicated in the beginning. Even in association with rakta-pitta, unction measure is not regarded as beneficial in the beginning.
- In vataja visarpa and paittika visarpa of mild aggravated dosha, tiktaka ghritam is beneficial. But if the pitta dosha is excessively aggravated then virechana should be given.
- In the condition of excessively aggravated dosha, ghee should not be given at first, which does not cause virechana. Because non purgating ghee occlude the dosha resulting in decomposed skin, flesh and blood. Hence in visarpa, virechana followed by raktamokshana is recommended because the disorder is located in blood.
- If dosha in shakha (body elements) vitiate the blood, then raktamokshana should be administered first. The physician should use vishana (deer horn) in vata dominance, jalauka (Hirudinea medicinalis) in pitta dominance and alabu (lagenaria siceraria) in kapha dominance for blood letting or physician should perform siravyadha (blood letting through vein) promptly from the adjacent vein to the affected part, without which rakta kleda (putrifying blood content) gives rise to decomposed skin, flesh and ligaments.
- External application in the form of pralepa, pradeha and alepana (local applications of pastes) are to be used repeatedly for treatment of external lesions in visarpa. The guidelines shall be followed for local applications.
- Diet articles with sweet, bitter, cooling and blood pacifying properties is prescribed in the treatment of visarpa.
- Vidahi (that causes burning) and viruddha (mutually contradictory or incompatible) diet, day sleep, anger, exercise, exposure to sun heat, fire and fast winds are contraindicated in visarpa.
- Predominantly shita (cool) measures are prescribed in pitta dominant condition, ruksha in kapha dominant condition and snigdha in vata dominant condition of visarpa. In agni visarpa, vata-pitta pacifying measures are beneficial and in kardama visarpa mostly kapha pitta alleviating measures should be administered.
- The granthi visarpa, on inspection is predominant in rakta pitta, the physician experienced in timely management should treat the case with rukshana (de-oleation), langhana (lightening therapy), seka (affusion), and pradeha (external application) of panchavalka, siramoksha (blood letting), jalauka (leech therapy), vamana (emesis therapy), virechana (purgation therapy) and kashaya- tikta (astringent and bitter) ghee preparations. After cleansing of body by vamana and virechana, rakta mokshana should be administered and the measures alleviating vata-kapha are beneficial.
- The same line of treatment of granthi should be applied for the treatment of kaphaja galganda. The vatika galaganda associated with kapha may be cured by regular use of ghee, milk and decoction preparations.
Vidhi Vimarsha (Applied Inferences )
Causative factors of visarpa in contemporary era
Modern point of view visarpa is generally caused by a variety of infections. As per Punarvasu Atreya, the general etiological factors of visarpa are diet and lifestyle, injury, poisons, toxins, burns etc; some of these cause vitiation of dosha and khavaigunya (disease prone condition) in dhatu and some cause direct vitiation of dosha and dhatu leading to visarpa. This is confusing to the new scholars. Atreya's understanding of etiology is more specific because favorable condition for infection occurs at first then infection therefore diet and lifestyle related factors are described in detail and in the beginning. In treatment plan this concept of favorable environment should be considered. Change in internal body environment is possible by shodhana therapy and aushadha along with treatment of infection.
Pathophysiology of Visarpa [flow chart]
Common clinical conditions considered under visarpa
Visarpa is acute and extensive spreading in nature. As kushtha is chronic in nature and visarpa is acute therefore spreading kushtha should not be interpreted as visarpa. It is observed that visarpa interpretation to allopath disorders is very confusing to the scholars. It is difficult to label visarpa as a single entity. For proper interpretation, experienced intelligent expert in emergency treatments is required and diagnostic research in this direction is challenge to the researchers.
Clinical manifestation of vatika visarpa suggests bahih-srita visarpa and generally observed in acute skin infections (erysipelas etc.) and is curable with prompt management.
Paittika visarpa symptoms are suggestive of severe skin disease (erysipelas, extensive herpes, burns etc.) and are curable with appropriate management.
Kaphaja visarpa appears as progressively but gradually spreading ailment, suggestive of acute skin infection (erysipelas etc.) and is curable.
Agni visarpa is a serious infection of skin and lead to septicemia like condition. Agnivisarpa with the signs and symptoms described here is a serious ailment and is incurable. This ailment may be cured if vitals are not involved.
The name kardam visarpa is because the affected part appears like kardam (mud). The clinical picture of kardam described here is serious skin infection, necrotizing the adjacent structures (Necrotizing Fasciitis, gangrene etc.) and is incurable. The curable variant should be considered agnivisarpa.
Granthi visarpa is a serious ailment (B cell lymphoma etc.) and associated with complications is incurable.
Sannipatik visarpa is a very serious manifestation of visarpa and is ubhaya-samsrita. This is like a very serious manifestation of sepsis and is not treatable.
Current clinical practices in management of visarpa
Experience based
Prognostic assessment of disease is very important while treating acute disorders. Majority of visarpa cases are having bad prognosis as per experience of Punarvasu Atreya. Even though some cases of curable bahihsrita visarpa may become incurable and fatal if not treated early and promptly. Quick diagnosis of life threatening conditions and prompt life saving management in intensive care unit is required in visarpa disorder.
It is already stated that there are serious diseases which are curable but they cause death if not treated. Agni and kardam visarpa are curable only by the most effective therapeutic measures. Antahsrita and ubhaysamsrita visarpa are incurable or sometimes may be cured by most experienced, intelligent physician with most appropriate timely approach in intensive care unit. Bahihsrita curable visarpa may convert into ubhayasamsrita if not treated appropriately.
Shodhana and shamana therapy is described for curable visarpa and maximum visarpa cases are incurable. This is challenge to the researchers to apply shodhana and shamana therapy in incurable emergency cases along with life saving management to cure the incurable ones.
Evidence based studies
Visarpa is acute and fatal in nature and maximum Ayurveda hospitals have limited facilities for emergency managements. Some of clinicians are treating self limiting minor cases of herpes as a visarpa following the treatment of pittaja visarpa. A case study on effect of Ayurvedic management in oro-facial herpes was conducted. The diagnosed case of oro-facial herpes in 72-year-old male patient was treated with medicines of bitter taste (tikta rasa) internally, diet regimen, anulomana variety of therapeutic purgation (virechana) and topical application of cold (sheeta)-dry(ruksha) medicines(lepa). The case is observed symptom free after a total period of 164 days.[1]
Researches done on visarpa
Considerable research work is not carried out on visarpa by Ayurveda researchers. This is due to acute and fatal nature of this disease and Ayurveda research centers are not well equipped for emergency managements. Hence it is necessary to work in the direction to treat such incurable fatal condition. Initially research work on this disease may be carried out in collaboration with well equipped intensive care unit and experts in emergency managements. Researchers may work by combining algorithmic Ayurveda treatment with allopath. Incurable and fatal cases of visarpa experienced by Punarvasu Atreya may be cured with early appropriate management in intensive care unit due to advances in drug research and technology.
Further reading
- Charak, Chikitsa Sthana, chap 21 Visarpa Chikitsa Adhyaya. In:Vaidya Yadavaji Trikamji Aacharya, Editor, Charak samhita, 2nd edition, Varanasi;Chaukhamba Sanskrit Sansthan,1990;228.
- Chakrapani,Charak,Chikitsa Sthana, Chap 21 Visarpa Chikitsa Adhyaya, 2nd edition,Varanasi; Chaukhamba Sanskrit Sansthan, 1990; 225.
- Charak,Cikitsa Sthana,Chap 21 Visarpa Cikitsitam. In: Pt. Dutta R, editor. Charak Samhita, 2nd ed., 2003 reprint, Varanasi: Chaukhambha Bharti Academy; 2003. p. 231.
- Charak,Chikitsa Sthana, Chap 21 Visarpa Chikitsa Adhyaya,In:Kashiram Shastri and Gorakhnath Chaturvedi, editors. Charak Samhita,(Hindi traslation) Part II. Varanasi: Chaukhambha Bharati Academy; Reprint 2005. p. 235.
- Charak, Chikitsa Sthana, Visarpa Cikitsitam,21, In: Vd. Khushvaha HS,editors,Charak Samhita Ayushi hindi commentary, 1 st edition, Chaukhambha Orientalia Publisher, Varanasi, 2009;224.
- Chakrapani, Charak, Cikitsa Sthana, Chap 21 Visarpa Cikitsitam. In: Vd. Yadavaji T. A.,Editor, Charak Samhita, 1 st edition, Varanasi;Chaukhambha Orientalia Publications, 2001;227.
- Sushruta. Cikitsa Sthana, 17. Visarpanadisthanaroga Chikitsitam Adhyaya In: Vaidya Yadavji Trikamji Acharaya, Narayan Ram Acharaya, editors. Sushruta Samhita,?ed, Varanasi: Chaukhambha Orientalia; 2007. p. 321.
- Susruta, Nidana sthana,cha 10, Visarpanadisthanaroga Nidana In:Kaviraj Ambikadutt Shastri,editor, Sushruta Samhita, 11 th ed. Varanasi: Chaukhambha Sanskrit Sansthan; 1998. p. 129.
- Vagbhata, Ashtanga Sangraha, Cikitsa Sthana, 20,Visarpa chikitsitam Adhyaya. translated to English by Prof. Murthy KR, 9 th edition,Varanasi; Chaukhambha Orientalia Publisher,2005;229.
- Vagbhata, Ashtanga Sangraha, Nidana Sthana, 13, Pandurogakamalasophavisarpa Nidanam Adhyaya. translated to English by Prof. Murthy KR, 9 th edition, Varanasi,Chaukhambha Orientalia Publisher, 2005; 229.
- Vagbhata, Ashtanga Hridyam ,Cikitsa Sthana,18. Visarpa chikitsitam Adhyaya .Translated to English by Prof. K.R. Shrikanth Murthy, 7 th ed., Vol. 1. Varanasi: Chaukhambha Krishnadas Academy; 2010. p. 221.
- Vagbhata,Ashtanga Hridyam , Nidana Sthana, Chap 13 Pandurogasophavisarpa Nidana.Translated by Prof. K.R. Shrikanth Murthy, 7 th ed., Vol. 1. Varanasi: Chaukhambha Krishnadas Academy; 2010. p. 221.
Send us your suggestions and feedback on this page.
References
- ↑ Mutnali K, Roopa BJ, Shivaprasad T, Yadav R. Ayurveda management of oro-facial herpes: a case report. J Ayurveda Integr Med. 2020 Jul-Sep;11(3):357-359. doi: 10.1016/j.jaim.2020.06.003. Epub 2020 Aug 4. PMID: 32768346; PMCID: PMC7527852.