Pandu Chikitsa
Chikitsa Sthana Chapter 16. Management of Pandu (Anemia and diseases due to blood deficiency)
| Section/Chapter | Chikitsa Sthana Chapter 16 |
|---|---|
| Preceding Chapter | Grahani Chikitsa |
| Succeeding Chapter | Hikka Shwasa Chikitsa |
| Other Sections | Sutra Sthana, Nidana Sthana, Vimana Sthana, Sharira Sthana, Indriya Sthana, Kalpa Sthana, Siddhi Sthana |
| Translator and commentator | Kar A.C., Rai S., Aladoriya N., Deole Y. S. |
| Reviewer | Ojha S.N. |
| Editors | Singh G., Goyal M., Deole Y.S., Basisht G. |
| Year of publication | 2020 |
| Publisher | Charak Samhita Research, Training and Skill Development Centre |
| DOI | 10.47468/CSNE.2020.e01.s06.017 |
Abstract
Pandu roga (resembling with anemia) is characterized by pallor which is associated with different colors according to dosha involved. Besides pandu roga, this chapter also describes two types of kamala (jaundice) which are two other associated diseases, caused by predominance of pitta dosha which causes alteration in normal colors of the body. The chapter describes general etiology, pathogenesis, symptoms etc of pandu roga (anemia) as well as each of its five types viz. vata, pitta, kapha, sannipataja and mrittika-bhakshana (clay eating) pandu. After describing general principle of treatment of pandu and kamala, detailed treatment of each of the conditions mentioned above along with pathya (recommended diet) and apathya (prohibited diet) are given.
Keywords: Pandu roga, kamala, koshthashakhashrita kamala, shakhashrita kamala, panaka, kumbhakamala, haleemaka, anemia, jaundice
Introduction
After the description of grahani dosha, the chapter on pandu roga is given, as the causative factors of pandu roga are quite similar to that of grahani dosha. Probably it is because that the various gastrointestinal problems can also lead to development of pandu roga. The chapter deals with general discoloration of the body such as pallor, yellowish, greenish and whitish discoloration which is seen in skin, eyes, lips, face, nails, urine feces etc.
Kamala (jaundice) and haleemaka (severe obstructive jaundice) have also been included in this chapter as they are also characterized by the discoloration and may relate to pandu roga. Kamala is of two types, swatantra (primary) and partantra (secondary). The etiological factors of primary kamala are described later. Secondary kamala develops in chronic phase of pandu in which vitiated pitta is seated in rasa dhatu and in kamala, pitta goes deeper in rakta dhatu and continues to go deeper in mamsa dhatu and meda dhatu, then it is called haleemaka and kumbha kamala respectively.
Kamala is of two types in repect to location, shakhshrita kamala located in body tissues in the form of obstructed pitta and koshthashrita kamala, localized to gut and can be easily removed by purgation while shakhashrita kamala needs to be brought to gut for removal.
Sanskrit Text, Transliteration and English Translation
Now we shall expound the chapter "Pandu Chikitsa" (Management of Anemia and diseases due to blood deficiency). Thus said Lord Atreya. [1-2]
Five types of pandu
Pandu roga is classified into five types as vatika, paittika, kaphaja, tridoshaja and mrittika bhakshhana janya pandu [3]
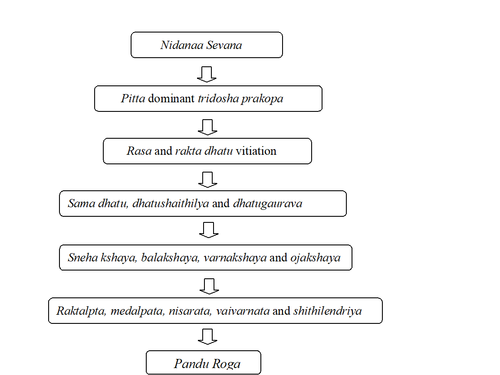
Pathogenesis of pandu
दोषाः पित्तप्रधानास्तु यस्य कुप्यन्ति धातुषु|
शैथिल्यं तस्य धातूनां गौरवं चोपजायते||४||
ततो वर्णबलस्नेहा ये चान्येऽप्योजसो गुणाः|
व्रजन्ति क्षयमत्यर्थं दोषदूष्यप्रदूषणात्||५||
सोऽल्परक्तोऽल्पमेदस्को निःसारः शिथिलेन्द्रियः|
वैवर्ण्यं भजते, तस्य हेतुं शृणु सलक्षणम्||६||
Aggravated pitta predominant dosha vitiates the dhatu. This vitiation of dhatu cause sluggishnesss (shithilata) and heaviness (gaurava) in the dhatu resulting in diminution of complexion (varna), strength (bala), unctuousness (sneha) and the qualities of ojas. Thus, the person develops diminished blood (rakta) and the fatty tissue (meda dhatu) and absence of the vitality of all the tissues (nihsara) decreases functional status of sense organs (sithilendriyah) and discoloration of the body. Hetu (etiological factors and pathogenesis) and the sign and symptoms of the disease will be explained hereafter [4-6]
General etio-pathogenesis of pandu
क्षाराम्ललवणात्युष्णविरुद्धासात्म्यभोजनात्|
निष्पावमाषपिण्याकतिलतैलनिषेवणात्||७||
विदग्धेऽन्ने दिवास्वप्नाद्व्यायामान्मैथुनात्तथा|
प्रतिकर्मर्तुवैषम्याद्वेगानां च विधारणात्||८||
कामचिन्ताभयक्रोधशोकोपहतचेतसः|
समुदीर्णं यदा पित्तं हृदये समवस्थितम्||९||
वायुना बलिना क्षिप्तं सम्प्राप्य धमनीर्दश|
प्रपन्नं केवलं देहं त्वङ्मांसान्तरमाश्रितम्||१०||
प्रदूष्य कफवातासृक्त्वङ्मांसानि करोति तत्|
पाण्डुहारिद्रहरितान् वर्णान् बहुविधांस्त्वचि||११||
स पाण्डुरोग इत्युक्तः ...|१२|
Followings are the etiological factors of pandu:
- The (excessive) intake of alkaline, sour, saline, hot and mutually contradictory foods, unwholesome food, nishpava (a type of pulses), masha, pinyaka (oil cake) and tila oil;
- Indulging in day sleep, performing exercise and sex before digestion of the food;
- Improper administration of Panchakarma measures (pratikarma vaishamya) and the disobedience of the seasonal regimens (ritu vaishamya)
- Suppression of the natural urges
- Affliction of mind with passion, worry, fear, anger, grief
Indulgence in the above factors aggravates pitta seated in the cardiac region and then this pitta is forcefully propelled by the vata into the ten dhamanis (attached to the heart) and further into the whole body. There, it gets located in between the tvacha (skin) and the mamsa dhatu (flesh) and additionally vitiates the kapha, vata, rakta, tvacha and mamsa dhatu resulting in the development of various discolorations in the body like pandu (pale), haridra (yellow),and harita (green). This is called as pandu roga [7-11½]
Premonitory symptoms
The premonitory symptoms of the disease are palpitations, ununctuousness, absence of sweating and fatigue [12]
General symptoms of pandu
सम्भूतेऽस्मिन् भवेत् सर्वः कर्णक्ष्वेडी हतानलः|
दुर्बलः सदनोऽन्नद्विट् श्रमभ्रमनिपीडितः||१३||
गात्रशूलज्वरश्वासगौरवारुचिमान्नरः|
मृदितैरिव गात्रैश्च पीडितोन्मथितैरिव||१४||
शूनाक्षिकूटो हरितः शीर्णलोमा हतप्रभः|
कोपनः शिशिरद्वेषी निद्रालुः ष्ठीवनोऽल्पवाक्||१५||
पिण्डिकोद्वेष्टकट्यूरुपादरुक्सदनानि च|
भवन्त्यारोहणायासैर्विशेषश्चास्य [१] वक्ष्यते||१६||
On developing pandu roga the patients have the symptoms of tinnitus, low digestion, weakness, prostration, disliking for food, fatigue, giddiness, pain in the body, fever, dyspnea, heaviness and anorexia. The patient feels as if the limbs are being kneaded, pressed or churned; develops peri-orbital swelling, greenish complexion and falling of body hair. The person loses his body luster, becomes irritable, dislikes cold things, feels sleepy, spits in excess, avoids speaking, suffers from cramps in the calf region and experiences excessive fatigue as well as pain and weakness in the lumbar region, thighs and feet specifically by exertion while climbing [13-16]
The signs and symptoms specific to each variety of pandu will be described henceforth.
Vatika pandu
आहारैरुपचारैश्च वातलैः कुपितोऽनिलः|
जनयेत्कृष्णपाण्डुत्वं [१] तथा रूक्षारुणाङ्गताम्||१७||
अङ्गमर्दं रुजं तोदं कम्पं पार्श्वशिरोरुजम्|
वर्चःशोषास्यवैरस्यशोफानाहबलक्षयान्||१८||
Indulging in vata increasing diet and regimens aggravates vata leading to vatika pandu roga. The skin of the patient becomes blackish dawn colored and ununctuous. Its other symptoms are malaise, ache, pricking pain, tremor, pain in both the sides of the chest, headache; dried feces, distaste in the mouth; swelling, gaseous distention of the abdomen and weakness [17-18]
Paittika pandu
पित्तलस्याचितं पित्तं यथोक्तैः स्वैः प्रकोपणैः|
दूषयित्वा तु रक्तादीन् पाण्डुरोगाय कल्पते||१९||
स पीतो हरिताभो वा ज्वरदाहसमन्वितः|
तृष्णामूर्च्छापिपासार्तः [१] पीतमूत्रशकृन्नरः||२०||
स्वेदनः शीतकामश्च न चान्नमभिनन्दति|
कटुकास्यो न चास्योष्णमुपशेतेऽम्लमेव च||२१||
उद्गारोऽम्लो विदाहश्च विदग्धेऽन्नेऽस्य जायते|
दौर्गन्ध्यं भिन्नवर्चस्त्वं दौर्बल्यं तम एव च||२२||
Pitta gets aggravated by indulging in pitta vitiating nidanas (diet and regimens) which by involving the blood etc. causes pittaja pandu. Its symptoms are, change in complexion to yellowish/greenish, fever, burning sensation; morbid thirst and fainting; excessive perspiration and longing for cold things and environment. The person does not relish food, develops pungent taste, disfavors hot and sour things; gets sour eructations associated with burning sensation due to impaired digestion of food; emits foul smell from mouth; the urine and stool become yellow in color, has loose motions and develops weakness and fainting [19-22]
Kaphaja pandu
विवृद्धः श्लेष्मलैः श्लेष्मा पाण्डुरोगं स पूर्ववत्|
करोति गौरवं तन्द्रा छर्दिं श्वेतावभासताम्||२३||
प्रसेकं लोमहर्षं च सादं मूर्च्छां भ्रमं क्लमम्|
श्वासं कासं तथाऽऽलस्यमरुचिं वाक्स्वरग्रहम्||२४||
शुक्लमूत्राक्षिवर्चस्त्वं कटुरूक्षोष्णकामताम्|
श्वयथुं मधुरास्यत्वमिति [१] पाण्ड्वामयः कफात्||२५||
Aggravated kapha by indulging in kapha increasing diet and regimen gives rise to kaphaja pandu roga through the pathogenesis described earlier. The sign and symptoms of kaphaja pandu are heaviness, drowsiness, vomiting, whitish complexion, salivation, horripilation, prostration, fainting, giddiness, mental fatigue, dyspnea, cough, laziness, anorexia, obstruction in speech and voice, whitish coloration of the eyes, urine and feces; longing for pungent, ununctuous and hot things; and develops edema and sweet taste in the mouth [23-25]
Tridoshaja pandu
सर्वान्नसेविनः सर्वे दुष्टा दोषास्त्रिदोषजम्| त्रिदोषलिङ्गं कुर्वन्ति पाण्डुरोगं सुदुःसहम्||२६||
Indulging in the etiological factors of all the three types of pandu leads to aggravation of the three dosha resulting in tridoshaja pandu with the features of all the three types of pandu roga. This type of pandu causes much distress to the patient [26]
Mrittika bhakshana pandu
मृत्तिकादनशीलस्य कुप्यत्यन्यतमो मलः| कषाया मारुतं, पित्तमूषरा, मधुरा कफम्||२७||
कोपयेन्मृद्रसादींश्च रौक्ष्याद्भुक्तं विरूक्षयेत् [१] | पूरयत्यविपक्वैव स्रोतांसि निरुणद्धि च||२८||
इन्द्रियाणां बलं हत्वा तेजो वीर्यौजसी तथा| पाण्डुरोगं करोत्याशु बलवर्णाग्निनाशनम्||२९||
शूनगण्डाक्षिकूटभ्रूः [२] शूनपान्नाभिमेहनः| क्रिमिकोष्ठोऽतिसार्येत मलं सासृक् कफान्वितम्||३०||
Person indulging in the habitual consumption of clay (mrittika) gets dośhā aggravated according to the taste of mud viz. astringent mud aggravates vata, saline and alkaline mud aggravates pitta and sweet mud aggravates kapha dosha. The clay further because of its ununctuousness causes dryness in the rasa (nutrients of the digested food). The clay due to its undigestable nature fills and blocks the channels of circulation leading to decrease in the sharpness of the senses, luster, energy and ojas (vital essence of the tissues). This quickly manifesting pandu results in the loss of strength, complexion and digestive power. Its clinical features are edema of the cheeks, peri orbital edema and edema on the eyebrows area, feet, umbilical region and the pudendum; infestation of worms in the koshtha (gastrointestinal tract) and loose motions, the stool associated with blood and mucus [27-30]
Prognosis of pandu
पाण्डुरोगश्चिरोत्पन्नः खरीभूतो न सिध्यति| कालप्रकर्षाच्छूनो [१] ना यश्च पीतानि पश्यति||३१||
बद्धाल्पविट्कं सकफं हरितं योऽतिसार्यते| दीनः श्वेतातिदिग्धाङ्गश्छर्दिमूर्च्छातृषार्दितः||३२||
स नास्त्यसृक्क्षयाद्यश्च पाण्डुः श्वेतत्वमाप्नुयात्| इति पञ्चविधस्योक्तं पाण्डुरोगस्य लक्षणम्||३३||
Chronic pandu roga is incurable. Other symptoms indicating the incurability are appearance of excessive dryness and edema; patient visualizes everything as yellow; passes very hard stool or less amount of stool or passes loose stool associated with mucus and green in color; feels exceedingly prostrated; body becomes excessively white as if be smeared with whiteness; has vomiting, fainting and excessive thirst and when the patient develops excessive whiteness in the body as a result of loss of blood.
Thus, the signs and symptoms of all the five type of pandu roga have been described [31-33]
Koshthashakhashraya kamala
पाण्डुरोगी तु योऽत्यर्थं पित्तलानि निषेवते| तस्य पित्तमसृग्मांसं दग्ध्वा रोगाय कल्पते||३४||
हारिद्रनेत्रः स भृशं हारिद्रत्वङ्नखाननः| रक्तपीतशकृन्मूत्रो भेकवर्णो हतेन्द्रियः||३५||
दाहाविपाकदौर्बल्यसदनारुचिकर्षितः| कामला बहुपित्तैषा कोष्ठशाखाश्रया मता||३६||
If a patient of pandu roga excessively follows pitta vitiating diet and regimen, the pitta so aggravated by involving the rakta and the mamsa dhatu causes kamala. Its clinical features are the eyes, skin, nails and face of the patient become exceedingly yellow; stool and urine become reddish-yellow in color; complexion develops a color similar to that of a frog (found in rainy season); the senses get impaired; has burning sensation, indigestion, weakness, prostration and anorexia. This kamala is caused by excess of pitta is known as koshthashakhashrita [34-36]
Kumbha kamala
कालान्तरात् खरीभूता कृच्छ्रा स्यात् कुम्भकामला| 36½ |
With the due course of time the disease (kamala) becomes deep seated (kharibhuta) resulting in excessive dryness of the body or afflicted tissue and thus becomes difficult to cure. This condition is called kumbha kamala [36½]
Bad prognostic symptoms of kamala
कृष्णपीतशकृन्मूत्रो [१] भृशं शूनश्च मानवः||३७||
सरक्ताक्षिमुखच्छर्दिविण्मूत्रो यश्च ताम्यति| दाहारुचितृषानाहतन्द्रामोहसमन्वितः||३८||
नष्टाग्निसञ्ज्ञः क्षिप्रं हि कामलावान् विपद्यते|38½|
If the stool and urine of the patient (of kamala) become black and yellow; develops excessive edema; eyes and face becomes red colored; vomit, stool and urine are mixed with blood; the patient feels like going in darkness; has burning sensation, anorexia, morbid thirst, constipation, drowsiness and fainting; and the person looses his agni and consciousness; such patient may succumb to death quickly [37-38½]
Principles of treatment
साध्यानामितरेषां तु प्रवक्ष्यामि चिकित्सितम्||३९||
तत्र पाण्ड्वामयी स्निग्धस्तीक्ष्णैरूर्ध्वानुलोमिकैः| संशोध्यो मृदुभिस्तिक्तैः कामली तु विरेचनैः||४०||
ताभ्यां संशुद्धकोष्ठाभ्यां पथ्यान्यन्नानि दापयेत्| शालीन् सयवगोधूमान् पुराणान् यूषसंहितान्||४१||
मुद्गाढकीमसूरैश्च जाङ्गलैश्च रसैर्हितैः| यथादोषं विशिष्टं च तयोर्भैषज्यमाचरेत्||४२||
पञ्चगव्यं महातिक्तं कल्याणकमथापि वा| स्नेहनार्थं घृतं दद्यात् कामलापाण्डुरोगिणे||४३||
Now, the treatment for the curable types of pandu roga is being described here:
The patient suffering from the pandu should first be given strong (tikshna) emetic and purgation therapies after the administration of internal oleation (snehana) for cleansing of the body (shodhana).
On the other hand, patient of kamala should be given mild purgation therapy with bitter drugs. After the cleansing of the koshtha by the above procedures the patient of both of these diseases should be given wholesome food consisting of old shali rice, barley and wheat mixed with the yusha (vegetable soup) of mudga, adhaki and masura, and the rasa (meat soup) of animals inhabiting the arid zone.
On the basis of the aggravated dosha specific medicines are to be administered to the patients of these two categories (which will be described later in the chapter). For the oleation of the patient of pandu and kamala panchagavya ghrita, mahatikta ghrita and kalyanaka ghrita should be given [39-43]
Dadimadya ghritam
दाडिमात् कुडवो धान्यात् कुडवार्धं पलं पलम्| चित्रकाच्छृङ्गवेराच्च पिप्पल्यष्टमिका तथा||४४||
तैः कल्कैर्विंशतिपलं घृतस्य सलिलाढके| सिद्धं हृत्पाण्डुगुल्मार्शःप्लीहवातकफार्तिनुत्||४५||
दीपनं श्वासकासघ्नं मूढवाते च शस्यते| दुःखप्रसविनीनां च वन्ध्यानां चैव गर्भदम्||४६||
इति दाडिमाद्यं घृतम्|
Take twenty pala of ghee, one adhaka of water and add to it the paste prepared of one kudava of dadima, half kudava of dhanya, one pala each of chitraka and sringavera and one ashtamika (two karsha) of pippali and prepare ghee as per method of sneha paka.This medicated ghee stimulates the power of digestion. It cures heart disease, anemia, gulma, hemorrhoids, spleenomegaly and disorders of vata and kapha.It is also useful for curing asthma, bronchitis, mudha-vata (claudication of vata) and duhkha-prasava (difficult labor). It also helps a sterile woman to get offspring.
Thus, ends the description of dadimadyaghrita [44-46]
Katukadyam ghritam
कटुका रोहिणी मुस्तं हरिद्रे वत्सकात् पलम्| पटोलं चन्दनं मूर्वा त्रायमाणा दुरालभा||४७||
कृष्णा पर्पटको निम्बो भूनिम्बो देवदारु च| तैः कार्षिकैर्घृतप्रस्थः सिद्धः क्षीरचतुर्गुणः||४८||
रक्तपित्तं ज्वरं दाहं श्वयथुं स भगन्दरम्| अर्शांस्यसृग्दरं चैव हन्ति विस्फोटकांस्तथा||४९||
इति कटुकाद्यं घृतम्|
One pala each of katukarohini, musta, haridra, daruharidra, vatsaka in paste form, one karsha of each of patola, chandana, murva, trayamana, duralabha, krishna, parpataka, nimba, bhūnimba, devadaru should be added to one prastha of ghrita and four prasthas of milk. This medicated ghee cures raktapitta, jwara, daha, svayathu, bhagandara, arsha, asrigadara and visphotaka. Thus described katukadya ghritam [47-49]
Pathya ghritam
पथ्याशतरसे पथ्यावृन्तार्धशतकल्कवान्| प्रस्थः सिद्धो घृतात् पेयः स पाण्ड्वामयगुल्मनुत्||५०||
इति पथ्याघृतम्|
The decoction of one hundred fruits of haritaki and the paste of fifty stalks of haritaki fruits should be added to one prastha of ghee and cooked. This medicated ghee cures pandu and gulma [50]
Danti ghritam
दन्त्याश्चतुष्पलरसे पिष्टैर्दन्तीशलाटुभिः| तद्वत्प्रस्थो घृतात्सिद्धः प्लीहपाण्ड्वर्तिशोफजित्||५१||
इति दन्तीघृतम्|
One prastha of ghee should be cooked by adding (one prastha of) the decoction of four palas of danti and the paste of the green fruits of danti. Intake of this medicated ghee cures pleeha (splenic disorders), pandu and edema [51]
Drakshaghritam
पुराणसर्पिषः प्रस्थो द्राक्षार्धप्रस्थसाधितः| कामलागुल्मपाण्ड्वर्तिज्वरमेहोदरापहः||५२||
इति द्राक्षाघृतम्|
One prastha of old ghee should be added to half a prastha of draksha and cooked. This medicated ghee cures kamala, gulma, pandu, jwara, meha (polyuria) and udara roga (generalized abdominal enlargement)[52]
Haridradi ghritam
हरिद्रात्रिफलानिम्बबलामधुकसाधितम्| सक्षीरं माहिषं सर्पिः कामलाहरमुत्तमम्||५३||
इति हरिद्रादिघृतम्|
Ghrita prepared with haridra, triphala, nimba, balā, madhuka and buffalo’s milk and ghee is an excellent cure for kamala [53]
Darvyadi ghritam
गोमूत्रे द्विगुणे दार्व्याः कल्काक्षद्वयसाधितः| दार्व्याः पञ्चपलक्वाथे कल्के कालीयके परः||५४||
माहिषात् सर्पिषः प्रस्थः पूर्वः पूर्वे परे परः|५५|
One prastha of buffalo’s ghee prepared by adding two prasthas of cow’s urine and the paste of two aksha of the paste of darvi as per sneha kalpana cures pandu roga.
One prastha of buffalo’s ghee prepared by adding with the decoction of five palas of darvi and the paste of kaleeyaka as per sneha kalpana cures kamala [54-55]
Preparations for pandu roga
स्नेहैरेभिरुपक्रम्य स्निग्धं मत्वा विरेचयेत्||५५||
पयसा मूत्रयुक्तेन बहुशः केवलेन वा| दन्तीफलरसे कोष्णे काश्मर्याञ्जलिना शृतम्||५६||
द्राक्षाञ्जलिं मृदित्वा वा दद्यात् पाण्ड्वामयापहम्| द्विशर्करं त्रिवृच्चूर्णं पलार्धं पैत्तिकः पिबेत्||५७||
कफपाण्डुस्तु गोमूत्रक्लिन्नयुक्तां [१] हरीतकीम्| आरग्वधं [२] रसेनेक्षोर्विदार्यामलकस्य च||५८||
सत्र्यूषणं बिल्वपत्रं पिबेन्ना कामलापहम्| दन्त्यर्धपलकल्कं वा द्विगुडं शीतवारिणा||५९||
कामली त्रिवृतां वाऽपि त्रिफलाया रसैः पिबेत्| विशालात्रिफलामुस्तकुष्ठदारुकलिङ्गकान्||६०||
कार्षिकानर्धकर्षांशां कुर्यादतिविषां तथा| कर्षौ मधुरसाया द्वौ सर्वमेतत् [३] सुखाम्बुना||६१||
मृदितं तं रसं पूतं पीत्वा लिह्याच्च मध्वनु| कासं श्वासं ज्वरं दाहं पाण्डुरोगमरोचकम्||६२||
गुल्मानाहामवातांश्च रक्तपित्तं च नाशयेत्| त्रिफलाया गुडूच्या वा दार्व्या निम्बस्य वा रसम्||६३||
शीतं मधुयुतं प्रातः कामलार्तः पिबेन्नरः| क्षीरमूत्रं पिबेत् पक्षं गव्यं माहिषमेव वा||६४||
पाण्डुर्गोमूत्रयुक्तं वा सप्ताहं त्रिफलारसम्| तरुजान् ज्वलितान्मूत्रे निर्वाप्यामृद्य चाङ्कुरान्||६५||
मातुलुङ्गस्य तत् पूतं पाण्डुशोथहरं पिबेत्| स्वर्णक्षीरी त्रिवृच्छ्यामे भद्रदारु सनागरम्||६६||
गोमूत्राञ्जलिना पिष्टं मूत्रे वा क्वथितं पिबेत्| क्षीरमेभिः शृतं वाऽपि पिबेद्दोषानुलोमनम्||६७||
हरीतकीं प्रयोगेण गोमूत्रेणाथवा पिबेत्| जीर्णे क्षीरेण भुञ्जीत रसेन मधुरेण वा||६८||
सप्तरात्रं गवां मूत्रे भावितं वाऽप्ययोरजः| पाण्डुरोगप्रशान्त्यर्थं पयसा पाययेद्भिषक्||६९||
After proper oleation of the patient with the internal administration of the above described medicated ghrita, the patient should be given frequent medication with the following recipes:
Milk with cow’s urine or milk alone or lukewarm infusion of danti sprinkled with the powder of one anjali of kashmarya or mixed with the paste of one anjali (handful) of draksha; all these drugs cure pandu roga in general.
The patient suffering from paittika pandu should take half pala of trivitta mixed with one pala of sugar;
Kaphaja type of pandu patient should take haritaki churna immersed in cow’s urine.
Kamala patient should take aragvadha along with the juice of sugarcane, vidari, amalaki to which sunthi, maricha, pippali and bilva leaves have been added; or may take the paste of half pala of danti mixed with one pala of jaggery along with cold water; or may take trivritta along with decoction of triphala.
Vishaladi phanta – One karsha each of vishala, haritaki, bibhitaka, amalaki, musta, kushtha, devadaru and kalingaka; half karsha of ativisha, two karsha of madhurasa (murva) should be made to a paste by triturating with lukewarm water and strained. The patient should take honey after taking this infusion. This phanta cures cough, dyspnea, fever, burning sensation, pandu roga, anorexia, gulma (lumps in abdomen), anaha (gaseous distention of the abdomen), amavata (joint disorders caused by ama), and raktapitta (bleeding disorders).
Other drugs which are useful for these ailments are as follows:
- Kamala patients should take the decoction of triphala, guduchi, devadaru, or nimba after cooling and adding honey in the morning.
- Pandu patient may take the milk or urine of either cow or buffalo for one fortnight.
- Pandu patient may drink the decoction of triphala along with cow’s urine for one week.
- Patient suffering from pandu and sopha (edema) should drink the liquid obtained by straining the paste of tender branches of matulunga set afire and then immersed in cow’s urine.
- Suvarnakshiri, trivritta, syama-trivritta, bhadradaru and nagara should be triturated by adding one anjali of cow’s urine or should be made to a decoction by adding cow’s urine. The above mentioned drugs may also be boiled with milk. The drinking of these drugs brings about the downward motion of the doshas causing pandu.
- Then again, the patient suffering from pandu roga should take a course of haritaki with cow’s urine (for seven days) and then should take food either with milk or sweetened meat soup, and
- Physicians should give lauha bhasma impregnated for seven nights with cow’s urine along with milk for the alleviation of pandu roga [55-69]
त्र्यूषणत्रिफलामुस्तविडङ्गचित्रकाः समाः| नवायोरजसो भागास्तच्चूर्णं क्षौद्रसर्पिषा||७०||
भक्षयेत् पाण्डुहृद्रोगकुष्ठार्शःकामलापहम्| नवायसमिदं चूर्णं कृष्णात्रेयेण भाषितम्||७१||
इति नवायसचूर्णम्|
Take sunthi, pippali, maricha, haritaki, bibhitaki, amalaki, musta, vidanga and chitraka in one part each and nine parts of lauha bhasma and mix together. Intake of this recipe along with honey and ghee cures anemia, heart diseases, kushtha (group of skin diseases), arsha (hemorrhoids) and kamala. This medicine propounded by krishnatreya is called navayasa churna [70-71]
Mandura vataka
गुडनागरमण्डूरतिलांशान्मानतः समान्| पिप्पलीद्विगुणां कुर्याद्गुटिकां पाण्डुरोगिणे||७२||
त्र्यूषणं त्रिफला मुस्तं विडङ्गं चव्यचित्रकौ| दार्वीत्वङ्माक्षिको धातुर्ग्रन्थिकं देवदारु च||७३||
एतान् द्विपलिकान्भागांश्चूर्णं कुर्यात् पृथक् पृथक्| मण्डूरं द्विगुणं चूर्णाच्छुद्धमञ्जनसन्निभम्||७४||
गोमूत्रेऽष्टगुणे पक्त्वा तस्मिंस्तत् प्रक्षिपेत्ततः| उदुम्बरसमान्कृत्वा वटकांस्तान् यथाग्नि ना||७५||
उपयुञ्जीत तक्रेण सात्म्यं जीर्णे च भोजनम्| मण्डूरवटका ह्येते प्राणदाः पाण्डुरोगिणाम्||७६||
कुष्ठान्यजीर्णकं शोथमूरुस्तम्भं कफामयान्| अर्शांसि कामलां मेहं प्लीहानं शमयन्ति च||७७||
इति मण्डूरवटकाः|
Mandura vataka – jaggery, shunthi, mandura and tila in one part each along with two parts of pippali should be triturated and made in the form of pills. This medicine is suitable for the treatment of the patients with pandu roga.
Shunthi, pippali, maricha, haritaki, bibhitaki, amalaki, musta, vidanga, chavya, chitraka, bark of daruharidra, makshika (copper pyrite), pippalimoola and devadaru in the quantity of two pala each should be made to powders separately.
Mandura bhasma which is dark in color like collyrium, should be cooked by adding eight times of cow’s urine and the powders of the above drugs should be mixed to this. Vatakas (large sized pills) of the size of udumbara should be made out of this combination. This should be taken by the patient in the appropriate doses according to his agni (power of digestion and metabolism) along with butter milk. The patient should take wholesome food after its digestion. These pills named as mandura vataka are the life givers for the patients of pandu. It also cures kushtha, ajeerna (indigestion), sotha (edema), urustambha (stiffening of the thighs), disease caused by aggravation of the kapha, arsha (hemorrhoids), kamala (jaundice), meha (polyuria) and pleeha (splenic diseases).
Thus ends the description of two types of mandura vataka.[72-77]
Tapayadi lauha
ताप्याद्रिजतुरूप्यायोमलाः पञ्चपलाः पृथक्| चित्रकत्रिफलाव्योषविडङ्गैः पलिकैः सह||७८||
शर्कराष्टपलोन्मिश्राश्चूर्णिता मधुनाऽऽप्लुताः| अभ्यस्यास्त्वक्षमात्रा हि जीर्णे हितमिताशिना||७९||
कुलत्थकाकमाच्यादिकपोतपरिहारिणा|८०|
Tapyadi yoga – Tapya, shilajatu, silver, mandura in the amount of five pala each should be added to one pala each of chitraka, haritaki, bibhitaka, amalaki, sunthi, pippali, maricha and vidanga; and eight pala of sugar. This recipe should be taken by the patient habitually (by a pandu rogi) in the dose of one karsha along with adequate amount of honey. After the digestion of this drug the patient should take wholesome food in small quantity and should avoid using kulattha, kakamachi etc. and pigeon meat [78-80]
Yogaraja
त्रिफलायास्त्रयो भागास्त्रयस्त्रिकटुकस्य च||८०||
भागश्चित्रकमूलस्य विडङ्गानां तथैव च| पञ्चाश्मजतुनो भागास्तथा रूप्यमलस्य च||८१||
माक्षिकस्य च शुद्धस्य लौहस्य रजसस्तथा| अष्टौ भागाः सितायाश्च तत्सर्वं सूक्ष्मचूर्णितम्||८२||
माक्षिकेणाप्लुतं स्थाप्यमायसे भाजने शुभे| उदुम्बरसमां मात्रां ततः खादेद्यथाग्नि ना||८३||
दिने दिने प्रयुञ्जीत जीर्णे भोज्यं यथेप्सितम्| वर्जयित्वा कुलत्थानि काकमाचीं कपोतकम्||८४||
योगराज इति ख्यातो योगोऽयममृतोपमः| रसायनमिदं श्रेष्ठं सर्वरोगहरं शिवम्||८५||
पाण्डुरोगं विषं कासं यक्ष्माणं विषमज्वरम्| कुष्ठान्यजीर्णकं मेहं शोषं श्वासमरोचकम्||८६||
विशेषाद्धन्त्यपस्मारं कामलां गुदजानि च|
इति योगराजः|
Yogaraja – harītaki, bibhitaki, amalaki, shunthi, pippali, maricha, chitraka moola (root) and vidanga in the amount of one part each; five parts each of shilajatu, raupya mala (silver), purified makshika and lauha bhasma; eight parts of sugar – all should be made to a fine powder and mixed with adequate amount of honey and kept in clean iron jar. This recipe should be taken by the patient in a quantity equal to a fruit of udumbara according to the power of digestion every day and should be given the desired food excluding kulattha, kakamachi etc. and pigeon meat; only after the digestion of the taken drug. This ambrosia like recipe is called yogaraja. It is an excellent rejuvenative recipe which cures all diseases and bestows auspiciousness. It specially cures pandu, poisoning, kasa, yakshma, vishama jwara (irregular fevers), ajeerna, meha, soshha, swasa, aruchi, apasmara (epilepsy), kamala and arsha.
Thus ends the description of yogaraja [80-86]
Various formulations
Shilajatu Vataka
कौटजत्रिफलानिम्बपटोलघननागरैः||८७||
भावितानि दशाहानि रसैर्द्वित्रिगुणानि वा| शिलाजतुपलान्यष्टौ तावती सितशर्करा||८८||
त्वक्क्षीरी पिप्पली धात्री कर्कटाख्या पलोन्मिता|
निदिग्ध्याः फलमूलाभ्यां पलं युक्त्या त्रिगन्धकम्|
चूर्णितं मधुनः कुर्यात् त्रिपलेनाक्षिकान् गुडान्| दाडिमाम्बुपयःपक्षिरसतोयसुरासवान्||९०||
तान् भक्षयित्वाऽनुपिबेन्निरन्नो भुक्त एव वा| पाण्डुकुष्ठज्वरप्लीहतमकार्शोभगन्दरान्||९१||
पूतिहृच्छुक्रमूत्राग्निदोषशोषगरोदरान् [१] | कासासृग्दरपित्तासृक्शोथगुल्मगलामयान्||९२||
ते च सर्वव्रणान् हन्युः सर्वरोगहराः शिवाः|
इति शिलाजतुवटकाः|
Shilajatu vataka – Eight pala of shilajatu impregnated for ten, twenty or thirty days with the decoction of fruit of kutaja, haritaki, bibhitaka, amalaki, nimba, patola, ghana and nagara. Eight pala of sugar and one pala each of tvakakshiri, pippali, dhatri and karkatashringi; half pala each of the fruit and root of nidigdhika and adequate powder of tvaka, ela and patra should be added to this shilajatu. Vataka (large sized pills) of one aksha each should be prepared by adding three pala of honey to this powder. These pills can be taken on either empty stomach or after having food. The patient should drink the juice of dadima (pomegranate), milk, meat soup of birds, water, alcohol, asava (medicated wine) after taking this medicine. It cures pandu, kushtha, jwara, pleeha, tamaka svasa, arsha, bhagandara (fistula in ano), puti (putrified ulcers), hridroga (heart diseases), shukra dosha (diseases of semen), mutra dosha (diseases of urine), and agni dosha (diseases of digestion), sosha (consumption), gara (poisoning), udara, kasa, asrigdara (menorrhagia), raktapitta (bleeding disorders), sotha, gulma, galamayana (diseases of the throats) and all types of vrana (wounds). It cures all types of diseases and bestows auspiciousness. Thus, ends the description of shilajatu vataka. [87-92]
पुनर्नवा त्रिवृद्व्योषविडङ्गं दारु चित्रकम्||९३||
कुष्ठं हरिद्रे त्रिफला दन्ती चव्यं कलिङ्गकाः| पिप्पली [२] पिप्पलीमूलं मुस्तं चेति पलोन्मितम्||९४||
मण्डूरं द्विगुणं चूर्णाद्गोमूत्रे द्व्याढके पचेत्| कोलवद्गुटिकाः कृत्वा तक्रेणालोड्य ना पिबेत्||९५||
ताः पाण्डुरोगान् प्लीहानमर्शांसि विषमज्वरम्| श्वयथुं ग्रहणीदोषं हन्युः कुष्ठं क्रिमींस्तथा||९६||
इति पुनर्नवामण्डूरम्|
Powder of one pala each of punarnava, trivritta, sunthi, pippali, maricha, vidanga, devadaru, chitraka, kushtha, haridra, daruharidra, haritaki, bibhitaka, amalaki, danti, chavya, kālingaka, pippalī, pippalimoola and musta; and forty pala of mandura bhasma (rust of iron) coked in two adhaka of cow’s urine and made in the form of gutika of the size of kola. These pills should be taken with butter milk. It cures pandu, pleeha, arsha, vishama jwara, sotha, grahanidosha (sprue syndrome, irritable bowel syndrome), kushtha and krimi (parasitic infestation). Thus, ends the description of punarnava mandura.[93-96]
Darvyadi leha and other two recipes
दार्वीत्वक् त्रिफला व्योषं विडङ्गमयसो रजः| मधुसर्पिर्युतं लिह्यात् कामलापाण्डुरोगवान्||९७||
तुल्या अयोरजःपथ्याहरिद्राः क्षौद्रसर्पिषा| चूर्णिताः कामली लिह्याद्गुडक्षौद्रेण वाऽभयाः||९८||
त्रिफला द्वे हरिद्रे च कटुरोहिण्ययोरजः| चूर्णितं क्षौद्रसर्पिर्भ्यां स लेहः कामलापहः||९९||
Powder of the bark of daruharidra, haritaki, bibhitaka, amalaki, pippali, sunthi, maricha, vidanga and lauha bhasma mixed with ghee and honey, taken as a linctus by the patients suffering from pandu and kamala.
Two other recipes – Patients suffering from kamala should take the powder of one part each of lauha bhasma, haritaki and haridra along with honey and ghee and may also take the linctus of the powder of abhaya prepared by mixing with jaggery and honey. [97-99]
Dhatryavaleha
द्विपलांशां तुगाक्षीरीं नागरं मधुयष्टिकाम्| प्रास्थिकीं पिप्पलीं द्राक्षां शर्करार्धतुलां शुभाम्||१००||
धात्रीफलरसद्रोणे चूर्णितं लेहवत् पचेत्| शीतं मधुप्रस्थयुतं लिह्यात् पाणितलं ततः||१०१||
हन्त्येष कामलां पित्तं पाण्डुं कासं हलीमकम्|
इति धात्र्यवलेहः|
Dhatryavaleha – Vanshalochana, sunthi, maduyashti powders, each in two pala; one prastha each of pippali and draksha; and half a tula of sugar crystal added with one drona of amalaki fruit juice and cooked till it changes into linctus form. One prastha of honey is added to it after it cools down. Intake of one panitala of this linctus cures kamala, pitta vikaras, pandu, kasa and haleemaka [100-101]
Mandura vatakah
त्र्यूषणं त्रिफला चव्यं चित्रको देवदारु च||१०२||
विडङ्गान्यथ मुस्तं च वत्सकं चेति चूर्णयेत्| मण्डूरतुल्यं तच्चूर्णं गोमूत्रेऽष्टगुणे पचेत्||१०३||
शनैः सिद्धास्तथा शीताः कार्याः कर्षसमा गुडाः| यथाग्नि भक्षणीयास्ते प्लीहपाण्ड्वामयापहाः||१०४||
ग्रहण्यर्शोनुदश्चैव तक्रवाट्याशिनः स्मृताः|
इति मण्डूरवटकाः|
Mandura Vataka-II: Shunthi, pippali, maricha, haritaki, bibhitaka, amalaki, chavya, chitraka, devadaru, vidanga, musta and vatsaka in one part each, made in the form of powder and added to equal quantity (12 parts) of mandura bhasma, should then be boiled by adding eight times of cow’s urine over mild fire. After the recipe cools pills of one aksha each should be prepared and taken according to the power of digestion. This cures pleeha, pandu, grahani, and arsha. The patient should take buttermilk and vatya (a roasted barley preperation) while taking this pill [102-104]
Gaudo arishta
मञ्जिष्ठा रजनी द्राक्षा बलामूलान्ययोरजः||१०५||
लोध्रं चैतेषु गौडः स्यादरिष्टः पाण्डुरोगिणाम्|
इति गौडोऽरिष्टः|
Manjishtha, rajani, draksha, bala moola (roots), lauha bhasma, and lodhra should be added to jaggery and processed according to the method prescribed for arishta. It is called gaudo-arishta and is useful for the patients suffering from pandu roga [105]
Beejakarishta
बीजकात्षोडशपलं त्रिफलायाश्च विंशतिः||१०६||
द्राक्षायाः पञ्च लाक्षायाः सप्त द्रोणे जलस्य तत्| साध्यं पादावशेषे तु पूतशेषे समावपेत्||१०७||
शर्करायास्तुलां प्रस्थं माक्षिकस्य च कार्षिकम्| व्योषं व्याघ्रनखोशीरं क्रमुकं सैलवालुकम्||१०८||
मधुकं कुष्ठमित्येतच्चूर्णितं घृतभाजने| यवेषु दशरात्रं तद्ग्रीष्मे द्विः शिशिरे स्थितम्||१०९||
पिबेत्तद्ग्रहणीपाण्डुरोगार्शःशोथगुल्मनुत्| मूत्रकृच्छ्राश्मरीमेहकामलासन्निपातजित्||११०||
बीजकारिष्ट इत्येष आत्रेयेण प्रकीर्तितः|
इति बीजकारिष्टः|
Beejaka taken in the amount of sixteen pala, twenty pala of triphala, five pala of draksha and seven pala of laksha are added to one drona of water and boiled till one fourth of water remains. Water should then be taken out by straining. One tula of sugar, one pala of honey and one pala powder of each of the shunthi, pippali, maricha, vyaghranakha, kramuka, elavaluka, madhuka and kushtha are added to the above made decoction and the potion be stored in a jar smeared with ghee kept inside a barley heap for ten nights during summer and for twenty nights in winter. Intake of this potion cures grahani, pandu, arsha, sotha, gulma, mutra krichha (dysuria), ashmari (stones in the urinary tract), meha, kamala and diseases caused by all the three dosha. This is called beejaka arishta and it was propounded by Atreya.
Thus, ends the description of beejaka arishta [106-110]
Dhatryarishta
धात्रीफलसहस्रे द्वे पीडयित्वा रसं तु तम्||१११||
क्षौद्राष्टांशेन संयुक्तं कृष्णार्धकुडवेन च| शर्करार्धतुलोन्मिश्रं पक्षं स्निग्धघटे स्थितम्||११२||
प्रपिबेन्मात्रया प्रातर्जीर्णे हितमिताशनः| कामलापाण्डुहृद्रोगवातासृग्विषमज्वरान्||११३||
कासहिक्कारुचिश्वासांश्चैषोऽरिष्टः प्रणाशयेत्|
इति धात्र्यरिष्टः
Dhatryarishta - Two thousand fruits of amalaki should be crushed and the juice extracted should be mixed with one eighth the quantity of honey, half kudava of pippali and half tula of sugar. It should then be kept in an earthern jar smeared with ghee for one fortnight. It should be taken in appropriate dose in the morning and the patient should take wholesome food in small quantity after the digestion of the drug. This arishta cures kamala, pandu, hridroga, vatarakta, vishama jwara, kasa, hikka, aruchi and svasa. Thus, ends the description of dhatrya arishta [111-113]
Medicated water
Water boiled with the drugs belonging to sthiradi group is useful for drinking and the preparation of foods for pandu rogi; while the patient of kamala should use the juice of draksha and amalaki rasa [114-115]
Principles of treatment according to dosha
पाण्डुरोगप्रशान्त्यर्थमिति प्रोक्तं महर्षिणा||११५||
विकल्प्यमेतद्भिषजा पृथग्दोषबलं प्रति| वातिके स्नेहभूयिष्ठं, पैत्तिके तिक्तशीतलम्||११६||
श्लैष्मिके कटुतिक्तोष्णं [१] , विमिश्रं सान्निपातिके|११७|
The above mentioned drugs are described for the cure of pandu roga by the great sage (Punarvasu Atreya). The physician should make suitable changes (combinations and permutations) in the above depending upon the strength of the dosha in the patient.
The therapy should be dominated by unctuous drugs (oil, ghee etc) for vatika type of pandu; by bitter and cooling drugs for paittika type and by pungent, bitter and hot drugs for kaphaja type of pandu [115-117]
Treatment of mrittika bhakshanajanya pandu
निपातयेच्छरीरात्तु मृत्तिकां भक्षितां भिषक्||११७||
युक्तिज्ञः शोधनैस्तीक्ष्णैः प्रसमीक्ष्य बलाबलम्| शुद्धकायस्य सर्पींषि बलाधानानि योजयेत्||११८||
व्योषं बिल्वं हरिद्रे द्वे त्रिफला द्वे पुनर्नवे| मुस्तान्ययोरजः पाठा विडङ्गं देवदारु च||११९||
वृश्चिकाली च भार्गी च सक्षीरैस्तैः [१] समैर्घृतम्| साधयित्वा पिबेद्युक्त्या नरो मृद्दोषपीडितः||१२०||
तद्वत् केशरयष्ट्याह्वपिप्पलीक्षारशाद्वलैः| मृद्भक्षणादातुरस्य लौल्यादविनिवर्तिनः||१२१||
द्वेष्यार्थं भावितां कामं दद्यात्तद्दोषनाशनैः| विङ्गैलातिविषया निम्बपत्रेण पाठया||१२२||
वार्ताकैः कटुरोहिण्या कौटजैर्मूर्वयाऽपि वा|१२३|
A physician well versed in therapeutics, should give the patient strong elimination therapy, keeping in view the strength of the patient, in order to remove the swallowed mud from the body. After the body is cleansed, different types of medicated ghee should be prescribed to the patient for promotion of strength.
Ghee prepared with shunthi, pippali, maricha, bilva, haridra, daruharidra, haritaki, bibhitaka, amalaki, sveta and rakta punarnava, musta, lauha bhasma, patha, vidanga, devadaru, vrishchikali, bhargi and milk should be appropriately taken by the patient who suffers from anemia because of eating clay.
Likewise, ghee prepared with keshara, yashtamadhu, pippali, kshara (alkali preperation) and sadvala may be given to the patient suffering from mrittika bhakshana janya pandu.
If the patient is unable to give up his clay swallowing habits, he should be given clay impregnated with vidanga, ela, ativisha, neem leaves, patha, varataka, katurohiṇī, kutaja or murva with a view of creating an aversion to clay. These drugs also counter act the adverse effects of eating clay. [117-123]
Different types of treatment should be given to the patient suffering from mrittika bhakshana janya pandu, according to the different types of dosha aggravated. However, due to the specific type of etiological factor involved (clay eating), this type of pandu needs special type of treatment [123-124]
Shakhashrita kamala (kamala in body tissue with obstructive pathology)
तिलपिष्टनिभं यस्तु वर्चः सृजति कामली||१२४||
श्लेष्मणा रुद्धमार्गं तत् पित्तं कफहरैर्जयेत्| रूक्षशीतगुरुस्वादुव्यायामैर्वेगनिग्रहैः||१२५||
कफसम्मूर्च्छितो वायुः स्थानात् पित्तं क्षिपेद्बली| हारिद्रनेत्रमूत्रत्वक् श्वेतवर्चास्तदा नरः||१२६||
भवेत् साटोपविष्टम्भो गुरुणा हृदयेन च| दौर्बल्याल्पाग्निपार्श्वार्तिहिक्काश्वासारुचिज्वरैः||१२७||
क्रमेणाल्पेऽनुसज्येत [१] पित्ते शाखासमाश्रिते|१२८|
A patient of kamala if passes stools of the color of sesame paste (tila pishta nibhama), then it denotes obstruction in the passage of pitta by the kapha. Therefore, the pitta of such patient should be won by administration of drugs which also eliminate kapha.
The excess usage of ununctuous, cold and sweet ingredients; excessive exercise; suppression of the natural urges leads to the the aggravation of vata infilterated with kapha and the displacement of pitta from its site, resulting in the development of the following features:
The eyes, skin and urine of the patient become yellow while his stools become white in color. Additionally, the patients suffer from atopa (tympanitis), vishtambha (constipation associated with flatulence),and heaviness in the cardiac region, due to the displacement of pitta in the peripheral tissues (shakha), there is diminution in the flow of pitta (to the gastrointestinal tract) resulting in the gradual development of weakness, agnimandya (low digestion), parshva (pain in the sides of chest), hikka (hiccups), shvasa (dyspnea), aruchi (anorexia) and jwara [124-128]
Treatment of shakhashriat kamala
बर्हितित्तिरिदक्षाणां रूक्षाम्लैः कटुकै रसैः||१२८||
शुष्कमूलककौलत्थैर्यूषैश्चान्नानि भोजयेत्| मातुलुङ्गरसं क्षौद्रपिप्पलीमरिचान्वितम्||१२९||
सनागरं पिबेत् पित्तं तथाऽस्यैति स्वमाशयम्|१३०|
The patient suffering from from shakhashrita kamala should be given food along with the soup of the meat of peacock, tittira (partridge), daksha (rooster) sizzled with ununctuous, sour and pungent articles; and vegetable soups of dry mulaka (radish) and kulattha. The patient should also be given the juice of matulunga mixed with honey, pippali, maricha and shunthi for bringing the pitta to its own course [128-130]
कटुतीक्ष्णोष्णलवणैर्भृशाम्लैश्चाप्युपक्रमः||१३०||
आपित्तरागाच्छकृतो [१] वायोश्चाप्रशमाद्भवेत्| स्वस्थानमागते पित्ते पुरीषे पित्तरञ्जिते||१३१||
निवृत्तोपद्रवस्य स्यात् पूर्वः कामलिको विधिः|१३२|
Katu (pungent), teekshna (sharp), ushna (hot), lavana (saline) and extremely amla (sour) drugs should be continued till the stool of the patient acquires the color of pitta and the vata gets alleviated. When the pitta returns to its own habitat, the stool gets colored with pitta and the patient is relieved of complications, then further, the line of treatment described earlier for the treatment of kamala (koshthashrita) should be used [130-132]
Haleemaka (obstructive jaundice)
यदा तु पाण्डोर्वर्णः स्याद्धरितश्यावपीतकः||१३२||
बलोत्साहक्षयस्तन्द्रा मन्द्राग्नित्वं मृदुज्वरः| स्त्रीष्वहर्षोऽङ्गमर्दश्च श्वासस्तृष्णाऽरुचिर्भ्रमः||१३३||
हलीमकं तदा तस्य विद्यादनिलपित्ततः|१३४|
If a patient suffering from pandu develops green, black or yellow color and suffers from diminution of strength and enthusiasm; drowsiness, agnimandya (low digestion), mild fever, lack of libido (strisu aharsho), angamarda (malaise/ body ache), dyspnea, trishna (morbid thirst), anorexia and giddiness, the ailment is called haleemaka and is caused by the aggravation of vata and pitta dosha [132-134]
Treatment of haleemaka
गुडूचीस्वरसक्षीरसाधितं माहिषं घृतम्||१३४||
स पिबेत्त्रिवृतां स्निग्धो रसेनामलकस्य तु| विरिक्तो मधुरप्रायं भजेत् पित्तानिलापहम्||१३५||
द्राक्षालेहं च पूर्वोक्तं सर्पींषि मधुराणि च| यापनान् क्षीरबस्तींश्च शीलयेत्सानुवासनान्||१३६||
मार्द्वीकारिष्टयोगांश्च पिबेद्युक्त्याऽग्निवृद्धये| कासिकं चाभयालेहं पिप्पलीं मधुकं बलाम्||१३७||
पयसा च प्रयुञ्जीत यथादोषं यथाबलम्|१३८|
Patients suffering from haleemaka should take the recipe prepared from buffalo ghee by adding the juice of guduchi and milk.
After oleation with this oil the patient should take trivritta mixed with the juice of amalaki which causes purgation.
Thereafter food and drinks which are dominated by sweet taste and are alleviators of pitta and kapha should be given.
The patient should take drakshaleha described earlier (vide verse 100-102 in this chapter in the name of dhatryavaleha) and recipes of medicated ghee prepared by boiling with sweet drugs (vide verse 51-52). The patient should habitually indulge in taking different types of yapana basti (a type of medicated enema), kshara basti and anuvasana basti discussed in [ Cha. Sa. Siddhi Sthana ]. He should also take different recipes of arishta prepared from grapes (draksharishta) for the promotion of power of digestion. Abhaya leha described in the treatment of kasa [Cha. Sa. Chikitsa Sthana 18/57-62] may also be taken. Alternatively the patient may also take pippali, madhuka and bala along with milk depending upon the dosha aggravated and the strength of the patient [134-138]
Summary
तत्र श्लोकौ-
पाण्डोः पञ्चविधस्योक्तं हेतुलक्षणभेषजम्||१३८||
कामला द्विविधा तेषां साध्यासाध्यत्वमेव च|
तेषां विकल्पो यश्चान्यो महाव्याधिर्हलीमकः| तस्य चोक्तं समासेन व्यञ्जनं सचिकित्सितम्||१३९||
To sum up, the topics discussed in this chapter are:
- Five types of pandu along with the etiology, signs and symptoms; and treatment
- Two types of kamala and their curability as well as incurability
- Different varieties of kamala
- Haleemaka, which is a serious disease along with its signs and symptoms; and treatment [138-139]
इत्यग्निवेशकृते तन्त्रेऽप्राप्ते दृढबलसम्पूरिते चिकित्सास्थाने पाण्डुरोगचिकित्सितं नाम षोडशोऽध्यायः||१४0||
Thus ends the sixteenth chapter in Chikitsa Sthana dealing with the treatment of pandu roga in the work of Agnivesha which was redacted by Charaka and because of its unavailability was supplemented by Dridhabala [140]
Tattva Vimarsha (Fundamental Principles)
- The important pathological factors in pandu are aggravated three dosha with dominant pitta leading to slow metabolism at level of blood (rakta dhatu), the fatty tissue meda dhatu) and ojas qualities (affecting the vitality).
- The dietary factors like alkaline, sour, saline, hot and mutually contradictory foods, unwholesome food, nishpava (a type of pulses), masha, pinyaka (oil cake) and tila oil; lifestyle factors like indulging in day sleep, performing exercise and sex before digestion of the food, disobedience of the seasonal regimens (ritu vaishamya), suppression of the natural urges; iatrogenic factors like Improper administration of Panchakarma measures (pratikarma vaishamya) and the psychological factors like affliction of mind with passion, worry, fear, anger, grief are responsible for pandu.
- Heart and circulatory system are involved in the pathogenesis of pandu which is presented at the sites of skin and mamsa dhatu (flesh).
- The specific features are observed as per the dosha dominance in pathogenesis.
- Person indulging in the habitual consumption of clay (mrittika) gets dosha aggravated according to the taste of mud viz. astringent mud aggravates vata, saline and alkaline mud aggravates pitta and sweet mud aggravates kapha dosha. These factors cause pandu by affecting the dhatu and ojas.
- Chronic pandu roga is incurable. The prognosis depends upon involvement of [[dhatu] and its intensity.
- If a patient of pandu roga excessively consumes pitta vitiating diet and regimen, the aggravated pitta causes kamala by involving the rakta and the mamsa dhatu.
- First principle of management of pandu is administration of internal oleation (snehana) followed by strong (teekshna) emetic and purgation therapies for cleansing of the body (shodhana). In patients of kamala, mild purgation therapy with bitter drugs is advised.
- Kamala is of two types: Koshtha-shaksha shrita and shakhashrita. In koshtha-shakhashrita kamala there is excess increase in pitta.
- In shakhashrita kamala, pitta is obstructed by kapha and improperly circulated by vata. Therefore the treatment principles differ in both.
- In koshtha-shaksha shrita kamala, mild purgation is administered with bitter drugs with a focus on pacification ofpitta.
- In shakhashrita kamala, principles of management are pacification of kapha, and anulomana of vata to derive pitta to its own natural site. Therefore ruksha, amla, katu drugs are used in the treatment.
- Suitable changes (combinations and permutations) in the treatment should be prescribed depending upon the strength of the dosha in the patient. The therapy should be dominated by unctuous drugs (oil, ghee etc) for vatika type of pandu; by bitter and cooling drugs for paittika type and by pungent, bitter and hot drugs for kaphaja type of pandu.
- Strong elimination therapy is advised to remove the swallowed mud from the body after considering the strength of the patient. After the body is cleansed, different types of medicated ghee should be prescribed to the patient for promotion of strength.
- Haleemaka and is caused by the aggravation of vata and pitta dosha. Hence the treatment focus on pacification of vata and pitta dosha.
Vidhi Vimarsha (Applied Inferences )
Pathological factors
- Dosha: Pitta dominant three dosha, sadhaka and ranjak pitta, vyana and samana vata, avalambak and kledaka kapha
- Dhatu(vitiated factors): Rasa dhatu, rakta dhatu, mamsa dhatu and meda dhatu
- Status of agni/ dhatwagni/bhutagni: Manda at rasa dhatu, rakta dhatu, mamsa dhatu and meda dhatu level
- Origin of disease: Heart and channels, Liver and spleen
- Sites of vitiation: All body
- Sites of clinical presentation: All body specifically skin and subcutaneous tissues
- Srotas involved :Rasavaha, Raktavaha
- Type of samprapti : Avarodha and kshaya
- Basic principles of treatment: Shodhana (mainly virechana) and shamana (mainly pitta shamana) as per dosha dominance
General considerations
Pandu can be related with the disorders of improper formation of blood tissue due to vitiation of pitta dosha. Pitta dosha is considered to be responsible for all digestion, transformation and metabolism processes in the body. Therefore, the disorders like anemia, nutritional deficiency are mainly considered under pandu roga. The disorders which include pathologies of impaired metabolism and formation of plasma, blood, muscles and fat can also be referred under the umbrella of pandu roga. These include thyroid function disorders, hematological disorders like thalessemia, jaundice etc.
Etiological factors observed in present era
Diet
The dietary factors that cause vitiation of pitta dosha and poor nutritional status of rakta dhatu are enlisted to cause pandu. These include the items having sour, salt, pungent taste, hot potency, alkaline nature, mutually contradictory and unwholesome food. These shall be avoided to prevent pandu.
- Food with sour taste (amla ahara) includes sour curd, lemons, citric acid, pickles, and food with preservatives as jams, cold drinks, sauces, tamarind etc.
- Lavana ahara may be taken as food with excess salts or with salt added in packaged food or as pickles, chutneys etc.
- Madya includes alcoholic beverages as rum, beer, whisky, vodka etc.
- Kshara includes soda used in diet, cold drinks and beverages.
- Ati tikshna ahara includes as excessively spicy,pungent items as chhole, chaats, pakode, panipuri, chaaps, rajma, spicy vegetables and other dishes.
- Ati ushna includes food articles which are either very hot as tea, coffee etc. or which increase the metabolic activities of the body or also as very hot temperature.
- Mrittika bhakshana is considered as either oral ingestion of mud or use of articles contaminated with mud as unclean hands and fingers or as improperly washed vegetables or eatables.
- Asatmya bhojana may include food items that are not adopted or suited. It may be considered as sudden change of food style or habit or also as junk food used today, as they are not beneficial.
Some scientific studies have proven the role of some of the aharaja factors in the causation of panduroga as tea (considered as ati ushna nidana) has been proved to cause iron deficiency anemia by interfering with the absorption of iron. Similarly madya (alcohols) cause megaloblastic anemia by hampering the folate absorption.
Lifestyle
Excess day time sleep, exercise beyond one’s capacity and at improper time can lead to pandu. Therefore, proper quality sleep and proper exercise are preventive measures for pandu.
Psychological factors
Passion, worry, fear, anger and grief can affect digestion leading to poor nutritional status. Hence blissful state of mind is needed for proper nutrition. Rai and Kar in their observational study showed that worries, fear and grief are major etiological factors for iron deficiency anemia. These factors cause significant reduction of serum and bone marrow, while inhibiting the process of erythropoiesis. The inflammatory mediators such as IL-6, hepcidin are mediators in this pathology originated from grief and fear.[1]
Iatrogenic factors
Improper administration of oleation therapy and Panchakarma procedures can lead to pandu.
Pathophysiology
The cardinal feature of pandu is appearance of pallor on skin of the patient. Complexion and luster of skin is maintained by rasa dhatu and rakta dhatu. The texture is maintained by mamsa dhatu. Unctuousness is maintained by meda dhatu. These four dhatu are important for maintaining the natural appearance of skin. In pandu, the vitiated pitta, due to its hot and sharply acting properties, impairs digestion process at rasa dhatu, rakta dhatu, mamsa dhatu and meda dhatu leading to their poor formation. The rasa dhatu transport channels originate in the heart and its vessels. The origin of channels of rakta is in the liver and spleen. Therefore, symptoms related to cardio-vascular system and hematological system.
The sequential nourishment of rasa dhatu, rakta dhatu, mamsa dhatu and meda dhatu is impaired leading to poor quality tissues. Thus, overall functions of these systems are disturbed in pandu.
The type of pathogenesis includes formation of same dhatu (improperly formed tissues) due to poor digestive and metabolic processes at the above mentioned levels. Therefore, the treatment principle includes correction of this impairment.
Clinical features and conditions resembling the disease
Premonitory symptoms: Palpitations, dryness, lack of sweating, fatigue.
Signs: Decrease in complexion, strength, unctuousness and vitality are observed in pandu.
Various features related to that are categorized below:
| S.No. | Signs | Symptoms Manifested |
|---|---|---|
| 1 | Varnakshaya (depletion of complexion) | Discoloration of skin, poor lustre, pallor, yellowish, dark yellow skin |
| 2 | Balakshaya (depletion of strength) | Weakness, fatigue |
| 3 | Snehakshaya (depletion of unctuousness) | Dryness, poor quality of tissues |
| 4 | Ojakshaya (depletion of vitality) | Fearfulness, excess worries, impaired sensations, lack of concentration, poor appearance |
The following clinical features are observed in pandu. The involvement of dosha, dushya and channels are as given in the following table:
Signs
| S.No. | Signs | Dosha | Dushya | Srotas |
|---|---|---|---|---|
| 1 | Dhatushaithilya (laxity of tissues) | Pitta | Rasa dhatu | Rasavaha |
| 2 | Dhatu gaurava (heaviness in tissues) | Kapha | Rasa dhatu | Rasavaha |
| 3 | Varnakshaya (poor complexion) | Vata, Pitta | Rasa dhatu,Rakta dhatu | Rasavaha, Raktavaha |
| 4 | Balakshaya (poor strength) | Vata,Pitta | Rasa dhatu, Rakta dhatu | Rasavaha, Raktavaha |
| 5 | Snehakshaya (depletion of unctuousness) | Vata, Kapha | Rakta dhatu, Meda dhatu | Raktavaha, Medavaha |
| 6 | Ojagunakshaya (depletion of vitality) | Vata, Pitta | Sapta dhatu | Saptadhatu vaha |
| 7 | Raktalpata (poor quality and less blood) | Pitta | Rasa dhatu, Rakta dhatu | Rasavaha, Raktavaha |
| 8 | Medalpata (poor quality and less fats) | Vata, Pitta | Rakta dhatu, Mamsa dhatu | Raktavaha, Mamsavaha |
| 9 | Nihasarta (poor quality tissues) | Tridosha | Saptadhatu | Saptadhatu vaha |
| 10 | Shithilendriya (impairment of senses) | Tridosha | Saptadhatu | Rasavaha, Raktavaha |
| 11 | Vaivarnya (discoloration) | Pitta | Rasa dhatu,Rakta dhatu, Mamsa dhatu | Rasavaha, Raktavaha, Mamsavaha |
| 12 | Panduta (pallor) | Pitta | Rasa dhatu,Rakta dhatu, Mamsa dhatu | Rasavaha, Raktavaha, Mamsavaha |
Symptoms
| S.No. | Symptoms | Dosha | Dushya | Srotas |
|---|---|---|---|---|
| 1 | Karnakshweda (tinnitus) | Vata | Rakta dhatu | Raktavaha |
| 2 | Hatanala (poor digestion) | Kapha, Vata | Rasa dhatu | Rasavaha |
| 3 | Daurbalya (weakness) | Vata, Pitta | Saptadhatu | Rasavaha, Raktavaha |
| 4 | Sadana (bodyache) | Vata, Kapha | Rasa dhatu | Rasavaha |
| 5 | Annadwesha (anorexia) | Kapha | Rasa dhatu | Rasavaha |
| 6 | Shrama (overworked, fatigue) | Vata | Rasa dhatu | Rasavaha |
| 7 | Bhrama (vertigo) | Vata, Pitta | Majja dhatu | Majjavaha |
| 8 | Gatrashoola (pain) | Vata | Rakta dhatu, Mamsa dhatu | Raktavaha, Mamsavaha |
| 9 | Jwara (feverishness) | Pitta | Rasa dhatu, Sweda | Rasavaha, Swedavaha |
| 10 | Shwasa (dyspnea) | Vata, Kapha | Rasa dhatu | Rasavaha, Pranavaha |
| 11 | Gaurava (heaviness) | Kapha | Rasa dhatu | Rasavaha |
| 12 | Aruchi (aversion to food) | Kapha | Rasa dhatu | Rasavaha |
| 13 | Mridit iv gatrata (kneading pain) | Vata | Rasa dhatu, Rakta dhatu, Mamsa dhatu | Rasavaha, Raktavaha, Mamsavaha |
| 14 | Pidita unmathit gatrata (churning, pressing pain) | Vata | Rasa dhatu,Rakta dhatu, Mamsa dhatu | Rasavaha, Raktavaha, Mamsavaha |
| 15 | Akshikutashotha (pre-orbital swelling) | Kapha | Rasa dhatu | Rasavaha |
| 16 | Harita lomata (greenish body hair) | Pitta | Rasa dhatu | Rasavaha |
| 17 | Shirnalomata (falling body hair) | Vata,Pitta | Asthi dhatu | Asthivaha |
| 18 | Hatprabhatva (poor luster) | Pitta | Rakta dhatu | Raktavaha |
| 19 | Kopana (irritability) | Pitta | Rakta dhatu | Raktavaha |
| 20 | Shishiradwesha (disliking cold) | Vata | Rasa dhatu | Rasavaha |
| 21 | Nindraluta (excessive sleepiness) | Kapha | Rasa dhatu | Rasavaha |
| 22 | Sthivanadhikya (excessive sputum) | Kapha | Rasa dhatu | Rasavaha |
| 23 | Alpawaka (less speaking) | Vata | Rakta dhatu | Raktavaha |
| 24 | Pindikodweshtanam (pain in calf muscles) | Vata | Rakta dhatu,Mamsa dhatu | Raktavaha, Mamsavaha |
| 25 | Katiurupadaruka Sadana (pain in legs, thighs, and the lumbar region) | Vata | Rasa dhatu, Rakta dhatu, Mamsa dhatu | Rasavaha, Raktavaha, Mamsavaha |
| 26 | Arohaneayasa (dyspnea on climbing) | Vata, Kapha | Rasa dhatu | Rasavaha |
Differentiating features of dosha dominance
| Changes in color and texture manifested in the whole body and its parts | ||
|---|---|---|
| Vata dominant pandu | Pitta dominant pandu | Kapha dominant pandu |
| Blackish or dark reddish discoloration of the skin, blood vessels, nails, face and eyes | Yellowish discoloration of skin, the skin, blood vessels, nails, face and eyes | Whitishness discoloration of skin, the skin, blood vessels, nails, face and eyes |
| Features related to urine and stool | ||
| Blackish urine & stool, dry stools | Yellowish colored urine & stool, foul smelling and loose stools | Whitishness in the urine & stool |
| Features related to agni | ||
| Tastelessness in the mouth | Pungent taste in mouth | Sweet taste in the mouth |
| Abdominal distension | Does not relish food | Anorexia |
| Improper digestion of food | Heaviness | |
| Excessive salivation | ||
| Sour Eructation | Laziness | |
| Eructation associated with burning sensation | Vomiting | |
| Burning Sensation | ||
| Other features | ||
| Pain in the body, pricking pain | Increased body temperature | Drowsiness |
| Tremor | Excessive thirst | Horripilation |
| Headache | Fainting due to excessive thirst/coma | Mental fatigue |
| Weakness | Profuse sweating | Fainting |
| Pain in the sides of the chest | Weakness | Prostration |
| Giddiness | Inability to speak | |
| Swelling/Edema | Feeling of darkness in front of eyes | Cough, Dyspnea, Edema |
| Likings and Dislikings | ||
| Longing for cold things and environment | Likings for pungent items | |
| Dislike for hot food and atmosphere; also, do not suit the patient | Likings for ununctuous things | |
| Dislike for sour food; also, do not suit the patient | Likings for hot things | |
Consequences of dhatu kshaya
| S.No. | Pathological event | Consequence | Objectivity |
|---|---|---|---|
| 1 | Rasa dhatu kshaya | Decrease in quality tissue that nourish blood or required for formation of blood | Deficiency in factors required for erythropoietin like vitamin B12, Vitamin K, iron, transferin, ferritin, protein like hemochrome which give red color to blood, electrolyte Na+, K+, Ca++, Mg+, H+, Cl-, albumin, globulins, glucose, amino acid, nucleic acids and lipoprotein, endocrine secretions regulating fluid metabolism |
| 2 | Rakta dhatu kshaya | Decrease in quality and volume of blood and further decrease in factors required for formation of mamsa dhatu(muscles) | Decrease in volume of whole blood, hematocrit percentage, endocrine secretions regulating blood metabolism |
| 3 | Mamsa dhatu kshaya | Decrease in quality and volume of muscles and further decrease in factors required for formation of mamsa dhatu(muscles) | Decrease in muscle proteins, endocrine secretions regulating muscle metabolism |
| 4 | Meda dhatu kshaya | Decrease in quality and volume of fats and lipids and further decrease in factors required for formation of asthi dhatu(bones) | Decrease in lipids, endocrine secretions regulating lipid metabolism |
List of diseases with features as observed in pandu
| S.No. | Signs and Symptoms | Diseases |
|---|---|---|
| 1 | Blackish discoloration of the skin | Megaloblastic anemias (Vitamin B12 and folic acid deficiency) as reversible melanin skin hyperpigmentation which develops mainly over the knuckles |
| 2 | Reddish discoloration of body parts | Development of petechiae, echymosis or bruises on the body due to thrombocytopenia associated with anemia (as in Aplastic anemias). Anemia due to Addison’s disease (increased tanning) |
| 3 | Dry skin or body | Megaloblastic anemias due to the abnormal proliferation of epithelial cell surfaces. Anemia due to hypothyroid states |
| 4 | Reddish or Blackish discoloration in eyes, face and nails | Body parts due to spontaneous bleeding manifestations, pernicious anemia |
| 5 | Blackish urine | Cola colored urine in various types of intravascular hemolytic anemias when the plasma hemoglobin exceeds the haptoglobin binding capacity |
| 6 | Blackish stool/melena | Gastrointestinal bleeding responsible for anemias - may be due to any ulcers or worm infestations or any other cause |
| 7 | Dryness of stool or constipation | Megaloblastic anemias and anemia due to hypothyroidism |
| 8 | "Pins and needles" sensation | pernicious anemias as well as in megaloblastic anemias |
| 9 | Tremors | Cobalamin deficiency which causes peripheral neuropathy and degeneration of the posterior and pyramidal tracts of the spinal cord |
| 10 | Loss of taste/distaste | Pernicious anemia |
| 11 | Bodyache | Hemolytic anemia, hypothyroidism |
The observations of resemblance with diseases in conventional system of medicine show that all types of anemia specially megaloblastic anemia, pernicious anemia, hypothyroidism, haemolytic anemia can be considered under umbrella of pandu. The objective parameters used for these disorders can be utilized for research on efficacy of Ayurveda therapies in management of pandu.
Kamala
In the second part of the chapter pandu, kamala is elaborately described. If a person suffering from pandu follows pitta provoking diet and lifestyle, he suffers from kamala. This shows kamala is consequence of pandu or pandu is essential causative factor for kamala. This shows the relation of jaundice originated due to hemolytic anemia. In other types of jaundice, this notion is not observed in practice. Kamala can occur without pandu. (Su.Utt.44/9, A.Hri.Ni.13/15-17)
Yellowish discoloration of sclera, skin, face, nails, and urine associated with constitutional symptoms like anorexia, debility, indigestion, loss of physical strength is called Kamala.
Types of kamala
1. Shakhashrita Kamala/Alpa pitta (Dhatu ashrita)
The passage of pitta is obstructed by vitiated kapha and not allowing pitta to enter kostha, it will cause excess of pitta in body tissues in Shakhasrita Kamala. This involves the obstructive pathologies at hepatic circulation. As the pitta cannot enter the gastro-intestinal tract, it leads to clay colored stools. In obstructive jaundice, bilirubin has no access to the intestine and it is the reason for pale stools.
This description of stools being clay colored, but the urine being yellow shows that they were very close in concept to the modern day physiopathology of obstructive jaundice especially hepatocellular ones (wherein due to an inability of the bile to pass into the gastrointestinal tract it circulates into the blood and the conjugated bilirubin being water soluble fraction is filtered and passes out into the urine). Further the description of pitta being the bi-product of rakta is also very similar to the fact of bile being produced as a result of Red Blood Cell destruction. The most common cause is gall stones in the common bile duct and pancreatic cancer in the head of pancreas. Also, a group of parasites known as liver flukes can live in common bile duct causing obstructive jaundice. Biliary atresia, cholanjiocarcinoma, pancreatitis, cholestasis of pregnancy and pancreatic pseudocysts are causes for obstruction of bile flow into the duodenum.
2. Kostha Shakhashrita Kamala/bahu pitta (Maha Srotasashrita)
Bahupitta kamala or Kostha-shakhasrita kamala mostly resembles the pre-hepatic and hepatocellular jaundice. Pre-hepatic jaundice is caused by anything which causes haemolysis. Pre-hepatic cause include severe malaria, certain genetic diseases such as sickle cell anemia, spherocytosis, thalassemia, pyruvate kinase deficiency and glucose 6-phospate dehydrogenase (G6PD) deficiency, which lead to increased destruction of red cells and therefore hemolytic jaundice. Hepato-cellular Jaundice can be caused by acute or chronic hepatitis, hepatotoxicity, cirrhosis, drug induced hepatitis and alcoholic liver disease.
Haleemaka
Haleemaka is a further stage of pandu. Reduced oxygen carrying capacity of blood (reduced jeevan karma) causes depletion of strength and work capacity. This further leads to lack of libido and bodyache. Condition resembles cholestasis. Bile stasis and back pressure leads to liver failure which leads to the further symptoms of halimaka or sclerosing cholangitis. It is characterized by severe fatigue (bala utsaha hani), jaundice (harita pita meda), dark urine, cirrhosis, portal hypertension and hepato-megaly.
Panaki
Panaki, another disease in same context of halimaka, explains the condition of malabsorption especially of fat due to lack of bile juice in digestion due to obstruction which leads to steatorrhoea (bhinna varcha). Reduced fat absorption leads to deficiency of fat soluble vitamins such as A, D, E and K.
Kumbha Kamala
The description of kumbha kamala denotes the advanced stage of Kostha-shakhasrita kamala wherein the main seat of pathology is situated somewhere in the gastro-intestinal tract. Kumbha is one of the synonyms of koshtha. Edema is described as one of the important clinical features of kumbha kamala (Su. Utt. 44).
Both types of kamala, if not treated convert into difficult to treat and hardened skin. Kumbha kamala could also refer to the presentation of the patient having distended abdomen i.e. ascitis, which is one of the important clinical feature of liver diseases, which are also the main cause of jaundice.
Liver is the main seat for a number of functions and when it gets severely deranged the liver functions are affected. The clinical picture of kumbha kamala corresponds to these as observed below:
- The production of majority of proteins as albumin, few globulins, cerulo-plasmin etc., is hampered leading to edema in the various body parts (Bhrusham Shoonam cha Manavaḥ) and dryness in the body.
- The coagulation profile gets affected leading to increased prothrombin time, the presentation of esophageal varices, bleeding per rectum etc. Here the same features have been described as sarakta akshi mukha, chhardi vida mootra meaning blood seen or coming out of the eyes, mouth or in the vomitus (esophageal varices), through the stool (haemorrhoids) or through the urine.
- The derangement of liver structure in these diseases leads to some presentation of obstructive jaundice with yellow urine (peeta mootrata).
- The stage of altered consciousness has also been described as tandra moha samanvita (acting as if sleepy or having altered perception - semiconscious state).
- The stage of hepatic coma has also been described as nashta sangya means the person is not able to recognise and perceive anything – unconscious state (Sangya Nama Grahanena).
- The excessive dryness (kharibhuta) is generally due to increased bile salts deposition leading to pruritus and dryness of skin. This dryness further leads to the hardness.
- As liver disorders progress, coagulatory defects begin leading to upper G.I. track bleed causing black stools/malena(Krishna shakrita). Secondly conjugated bilirubin which does not enter intestine becomes urobilinogen giving urine dark color (krishna mutra).
- Excessive edema is observed all over body. Cirrhosis of the liver is a condition that causes reduction in plasma protein concentration. Cirrhosis means development of large amounts of fibrous tissue among the liver parenchymal cells. One result is failure of these cells to produce sufficient plasma proteins, leading to decreased plasma colloid osmotic pressure and the generalized edema that goes with this condition. Another way that liver cirrhosis causes edema is that the liver fibrosis sometimes compresses the abdominal portal venous drainage vessels as they pass through the liver before emptying back into the general circulation. Blockage of this portal venous outflow raises capillary hydrostatic pressure throughout the gastrointestinal area and further increases filtration of fluid out of the plasma into the intra-abdominal areas. When this occurs, the combined effects of decreased plasma protein concentration and high portal capillary pressures cause transudation of large amounts of fluid and protein into the abdominal cavity, a condition referred to as ascites.
- Hematemesis/bleeding in eyes,per rectum, hematuria (Sarakta akshi mukha chhardi vinamutra) explains the bleeding disorders which begin in late hepatic disorders.
- Fainting (tamah pravesha) is due to reduced cerebral perfusion due to various causes like gastrointestinal bleed, electrolyte or metabolic disturbance.
- Drowsiness (tandra), confusion (moha) are further symptoms of hepatic encephalopathy. Neuropsychological findings are experienced in all phases of hepatic encephalopathy. It is experienced as forgetfulness, mild confusion and irritability, inversed sleep pattern followed by lethargy and personality changes. The third stage is marked with worsened confusion and in fourth stage is coma. Mada, Murchha and sanyasa are mentioned earlier as disorders due to vitiated blood in Vidhishonitiya Adhyaya.
Management of Diseases (Treatment Protocols)
Current clinical practices in treatment of pandu and kamala ( referred from Chikitsa Pradeep)
| Type | Medicine | Dose | Time | Anupana |
|---|---|---|---|---|
| Vata dominant pandu | Mahayogaraja samira mixture | 120-480 mg | After meals | Ghee (dadimadi) + honey |
| Tiktaka ghritam | 10-40 ml | After meals | Hot water | |
| Navajivana rasa | 120-200 mg | After meals | Milk | |
| Pitta dominant pandu | Tapyadi lauha mixture | 250 - 600 mg | After meals | Dadimadi ghee + udumbaravaleha |
| Vasadi decoction | 20 - 40 ml | After meals | Honey | |
| Kapha dominant pandu | Gomutra Haritaki mixture | 600 mg - 3 grams | After meals | Honey + juice of castor leaves |
| Mrittika bhakshana janya | Gomutra Haritaki mixture | 600 mg - 3 grams | After meals | Kumari Asava |
| Riddha Patha Kamala | Ichha bhedi rasa | 120 - 180 mg | Early morning one time | Lemon juice |
| Suta shekhara kalpa | 120 - 250 mg | After meals | Milk + sugar | |
| Koshtha ashrita kamala | As like pitta dominant pandu | |||
Evidence based clinical practices
- In a study carried out by Shazi L. and Thakar A., Amalaki rasayana was found effective in management of iron deficiency anemia. However the efficacy was equal in clinical parameters and less in biochemical parameters in comparison to conventional drugs a combination of folic acid and ferrous sulphate. [2]
- Punarnava mandura was found effective as panduhara and rasayana in patients of geriatric anemia and can counteract most of the pathological manifestations related to pandu roga in old age (geriatric anemia)[3]. In another study on pregnant females, punarnava mandura and dhatri lauha are found effective in management of anemia during pregnancy.[4]
- A herbomineral formulation Trikatrayadi Lauha suspension was observed an effective, well-tolerated, and clinically safe formulation for the management of Iron deficiency anemia in children.[5] Khan et.al. observed that the same formulation was observed effective to relieve the signs and symptoms of pandu in comparison to standard control drug (Fersolate-CM). Trikatrayadi lauha provided significant improvement on Hbgm%, RBC, PCV, MCV, serum iron, percent transferrin saturation and to decrease TIBC. Therefore Trikatrayadi Lauha can be used in Panduroga or IDA as a safe hematinic drug.[6]
- Tewari et.al. studied the ethnopharmacological approaches to the therapy of jaundice[7] and highly used plant species from acanthaceae,euphorbiaceae, asteraceae, combretaceae and fabaceae family in the management of jaundice. The team of researchers elaborately studied hystorical perspective of jaundice, its pathophysiology and enlisted 207 herbs used in management of jaundice.[8]
Research studies on pandu
Some studies are available on the internet which depict the efficacy of various Ayurvedic drugs having iron (in the form of lauha and mandura) compounds in the management of pandu:
- Sarkar PK, Prajapati PK, Choudhary AK, Shukla VJ, Ravishankar B. Haematinic Evaluation of Lauha Bhasma and Mandura Bhasma on HgCl2-induced Anemia in Rats. Indian J Pharm Sci 2007;69:791-5.
- Sarkar PK. A Comparative Pharmaceutico-pharmaco-clinical study of Lauha Bhasma and Mandura Bhasma w.s.r. to its Pāndu-hara Effect, MD thesis. I.P.G.T. & R.A. Jamnagar: Gujrat Ayurveda University; 2005.
- Garai A, Rai M, Kumar A. Role of an Ayurvedic Compound (Panduhara Yoga) in the Management of Iron Deficiency Anaemia in Children. Ayu 2009;30:469-74.
- Gupta V, Reddy KR. Experimental Studies of Lohasava. Aryavaidyan 2007;21:87-94.
- Sarkar PK, Prajapati PK, Shukla VJ, Ravishankar B, Choudhary AK. Toxicity and recovery studies of two Ayurvedic preparations of iron. Indian J Exp Biol 2009;47:987-92.
- Devarshi P, Kanse A, Kanse R, Mane S, Patil S, Varute AT. Effect of Mandura Bhasma on lipolytic Activities of Liver, Kidney and Adipose Tissue of Albino Rat During CCl4 Induced hepatic Injury. J Biosci 1986;10:227-34.
- Pandit S, Biswas TK, Debnath PK, Saha AV, Chowdhury U, Shaw BP, et al. Chemical and pharmacological evaluation of different Ayurvedic preparations of iron. J Ethnopharmacology 1999;65:149-56.
- Dinesh C. Sharma, Deepa Chandiramani, Manminder Riyat and Praveen Sharma. Scientific evaluation of some ayurvedic preparations for correction of iron deficiency and anemia. Indian Journal of Clinical Biochemistry, 2007 / 22 (2) 123-128
- Ambika Das, PA03.17. A clinical evaluation of Punarnavadi Mandura and Dadimadi Ghritha in management of Pandu (Iron defeciency anaemia), Ancient Science of Life 2013; 32 (s2):86
One of the studies (Sharma D.C, 2007) report that the Ayurvedic preparations were found equally effective as the allopathic compound in the management of iron deficiency anemia and the fact that the side effects were almost nil establishes them to be even superior.
The modes of action of drugs and procedures as stated in this chapter, which is without iron, have not been studied much in anemia. Though, some of the preparations described in anemia have been found very useful in the management of other types of anemia as sickle cell anemia,[9] aplastic anemia,[10] etc.
So, further studies need to be done in order to know the efficacy of these drugs and mechanisms in the various types of anemia.
Principle of treatment for kamala
The management of kamala by the drugs stated in the chapter has been found to show good results but the mechanism of their action is still not clear. Practically few studies are available on the net which prove the efficacy of Ayurvedic compounds in the management of hepatocellular jaundice. [11]
List of Research Works done
IPGT&RA, Jamnagar
- Chaudhary sudhakar (1958): Pandu Roga Nidana.
- Mishra N. K. (1959): A clinical study of Pandu Roga.
- Bhattacharya R. C. (1965): Pandu Roga Par Paradamruta Teekshana Laugh Karyanvekshana
- Ojha N.H.(1966): Abhraka Bhasma Ka Pandu Roga Par Karyanvekshana.
- Pillai K.D.R. (1974): Study of effect of Swarna Makshika Bhasma on Pandu.
- Jha Prabhakar (1974): Swayama Lauha Bhasma Ka Pandu Roga Par Kriyatamaka Adhyayana.
- Sharada B.D.(1975) : Effect of Yogaraja on Garbhavasthajanya Pandu.
- Gopalkrishana (1986): Lauha Bhasma on Pandu with special reference to its Media.
- M.S.Trivedi (1992): Effect of Yogaraja Rasayana in Garbhavsthajanya Pandu.
- Nargunde Rajeshri (1997): A comparative Phaemaco-clinical Study of Shudha Kasisa Churna and Kasisa Bhasma on PANDU.
- Jain Sangeeta (2000): A study on Pandu Roga w.s.r. to ANAEMIA and Its Management with Shodhana and Yogaraja Rasayana.
- Sarkar P K (2005): A comparative pharmaco-pharmaceutico Clinical study of lauha bhasma and mandura bhasma w.s.r. to Panduhara effects.
Banaras Hindu University, Varanasi
- Trivedi R D (1979):Hematological and clinical stubby in pandu.
- Malhotra E. N. (1983): Management of Garbhavasthajnya Pandu with Mandura Bhasma.
- Nandkishore (1985): Clinical Assessment of Navayasa Lauha in Management of Pandu.
- Chauhana A. P. S. (1985): Role of Manduradi Ghanvati in Pandu Roga.
- Dixit A. K. (1994): Clinical study in Yogaraja Rasayana on Pandu.
- Singh S. N. (1996): A study on aetio pathogenesis of Pandu Roga w s r to its Samprapti Vighatan by Makshika.
- Agrawal N. Assessment of Effect of Mandura Bhasma in Iron Deficiency Anemia in Children, MD thesis. P.G. Department of Kaumarbhritya. Varanasi: IMS, B.H.U; 2007.
National Institute of Ayurveda, Jaipur and others
- Tyagi R. M. (1980): Pandu Roga Evam Vajra Vatak Mandura .
- B. C. Sharma (1985): Pandu Roga Samprapti Vivechana.
- R. K. Sharma (1994): Pandu Roga Mandura Bhasma Ka Chikitsatmaka Adhyayan.
- Meena R. K. (1994): Guduchi in Pandu Roga.
- Joshi N. (2005): Pharmaceutical, Pharmacological and Toxicological Study of Various Lauha Preparations(Kalpa) w.s.r. to Iron Deficiency Anaemia, M.D. Thesis. P. G. Department of Rasa Shastra and Bhaishajya Kalpana, Jaipur.
- Kumath V. (2006): A Comprehensive Study of Haritaki with Special Reference to the Efficacy of Terminalia chebula Retz. on pandu Roga, MD thesis. P. G. Department. of Dravyaguna, Government. Ujjain, Madhya Pradesh: Autonomous Dhanvantari Ayurveda College and Hospital; 2006.
Potential areas /scope for further research
The following drugs referred in management of pandu need to be researched more for providing evidences of its efficacy in anemia and related disorders in comparison to conventional management:
- Dadimadya ghritam
- Katukadyam ghritam
- Pathyaghritam
- Danti ghritam
- Drakshaghritam
- Haridradi ghritam
- Darvyadi ghritam
- Navayasa churnam
- Manduravataka
- Tapyadi lauha
- Yogaraja
- Punarnava Mandura
- Darvyadi leha
- Dhatryavaleha
- Manduravatakah
- Gaudo arishah
- Bijakarisha
- Dhatryarishta
Send us your suggestions and feedback on this page.
References
- ↑ Rai Shalini, Kar Anukul C. A review of role of psychological factors in the etiopathogenesis of Pandu roga with reference to iron deficiency anemia.Ayu,2016 Jan-March,31(1):18-21.
- ↑ Shaizi Layeeq, Thakar A.B. Clinical efficacy of Amalaki rasayana in the management of pandu(iron deficiency anemia). Ayu.2015.July-Sep.36(3):290-297.
- ↑ Pandya M.G. Dave A.R. A clinical study of punarnava mandura in the management of pandu roga in old age (geriatric anemia).Ayu,2014 July-Sept; 35(3);252-260.
- ↑ Khandelwal D.A, Donga S.B.,Dei L.P. Clinical efficacy of punarnava mandura and dhatri lauha in the management of garbhini pandu (anemia in pregnancy) Ayu,2015 Oct-Dec;36(4); 397-403.
- ↑ Kumar A, Garai AK. A clinical study on Pandu Roga, iron deficiency anemia, with Trikatrayadi Lauha suspension in children. J Ayurveda Integr Med 2012;3:215-22.
- ↑ Khan Subir kumar, Vyas S.N. Chandola H.M. Efficacy of Trikatrayadi lauha in Pandu roga with reference to iron deficiency anemia. Ayu 2012. Jan-Mar, 33(1):62-67.
- ↑ Tewari D, Mocan A, Parvanov ED, Sah AN, Nabavi SM, Huminiecki L, Ma ZF, Lee YY, Horba´nczuk JO and Atanasov AG (2017) Ethnopharmacological Approaches for Therapy of Jaundice: Part I. Front. Pharmacol. 8:518. doi: 10.3389/fphar.2017.00518
- ↑ Tewari D, Mocan A, Parvanov ED, Sah AN, Nabavi SM, Huminiecki L, Ma ZF, Lee YY, Horba´nczuk JO and Atanasov AG (2017) Ethnopharmacological Approaches for Therapy of Jaundice: Part II. Highly Used Plant Species from Acanthaceae, Euphorbiaceae, Asteraceae, Combretaceae, and Fabaceae Families. Front. Pharmacol. 8:519. doi: 10.3389/fphar.2017.00519
- ↑ Macmillan Keith, A herbomineral composition for the treatment of Sickle Cell disease. Retrieved from tgs.freshpatents.com
- ↑ Subhash singh, Shiv Kumar Singh and Narendra Kumar Singh. Aaplastic anaemia, complete cure, ayurvedic way – case report. International Journal Of Basic And Applied Medical Sciences Issn: 2277-2103 (Online) An Online International Journal Available At http://www.cibtech.org/jms.htm 2013 vol. 3 (1) january-april, pp.242-246/subhash et al.
- ↑ Nirmal kumar and Anil kumar singh. Phalatrikadi kvatha - an ayurvedic hepatoprotective drug. International journal of research in pharmacy and chemistry.2013, 3(3) Available online at www.ijrpc.com